What are the “Menopause Types” and why are they important?
As we explained in last week’s blog, Type 1 & Pre-menopause is where it all begins. Many women aren’t even aware of what’s happening “ or that anything is happening “ in the early part of Type 1. By the time she hits Type 2, she’s aware that something is happening, and she doesn’t care for it!
It’s important for every woman to know what’s happening in her body so she can respond appropriately. Can you imagine being 11 or 12 and having cramps and bleeding without knowing what a period is? Why should a woman in menopause be in the dark about the changes in her body?
Type 2: Stay calm and learn about your hormones
Every woman has the right to know where she is in the menopausal journey.
Especially the Type 2s. But because we don’t talk about menopause, women are frightened of what’s happening, thinking something is terribly wrong. It’s not, of course: it’s the utterly normal and natural process of menopause.
In Type 2, even though they’re in the thick of it, many women still don’t realize their physical and emotional changes are related to their hormones. If women are waiting for that first hot flash to tell them they’re in menopause, they may miss a lot of symptoms that can tell them sooner.
Also, some perimenopause symptoms “ in all types, but particularly in Type 2 “ can be truly frightening: anxiety risks, panic attacks, heart palpitations, flooding periods. Understanding that these happen can help so many women avoid unnecessary fear and ER visits and get to the right treatment faster.
Our Chief Medical Officer goes over the Symptoms and Science happening in Type 2 in this instructional video.
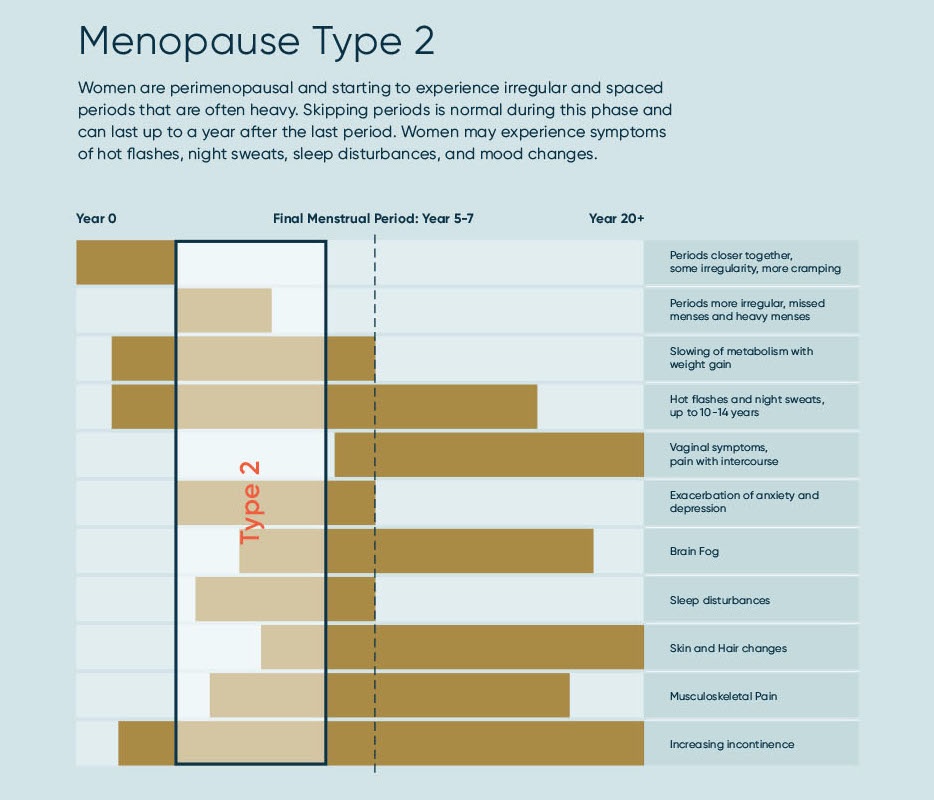
We created a “bird’s eye view” of where you are in your menopause journey and what to expect as to the ebb and flow of symptoms through the different menopause Types: where are you in your menopause journey.
Type 2 Symptoms
It’s no wonder women are confused: who would associate knee pain or heart palpitations with hormones? But because we have estrogen receptors all over our bodies, the effects of estrogen withdrawal are widespread, causing symptoms from brain fog to plantar fasciitis.
So let’s verify what Type 2 can look like as estrogen and progesterone start ramping downward.
Menopause Type 2s, your common pain points are:
- Irregular periods, often spaced farther apart, sometimes skipped, and probably heavier than usual.
- Further slowing of metabolism, with weight gain, often in the belly.
- Hot flashes start or may increase in frequency and intensity.
- Anxiety and depression can occur, reoccur, or worsen.
- Brain fog, memory lapse, and difficulty focusing can happen as there’s less estrogen to the brain.
- Sleep disturbances can start or increase.
- Skin and hair changes may begin with drying skin; brittle, thinning hair, and wrinkles.
- Joint pain increases, frequently showing up as knee and hip pain, pain in the hands, back pain, though pain can occur nearly anywhere.
- Increasing incontinence.
What to do about menopause in Type 2
First and foremost, start managing your symptoms. Type 2 is, in many ways, the most challenging phase with the greatest number of symptoms, often at their greatest intensity. Don’t just suffer! Since fatigue and sleeplessness are bad enough on their own and can make All The Things worse, we strongly suggest our Gennev AM/PM System. The multi-vitamin pack helps you have energy and balance during the day; and our sleep supports are formulated to help you fall asleep, stay asleep, and wake without anxiety.
Have you tried Jill’s Daily Vitamins for better sleep, focus, and energy?
Are you craving the energy you used to have? We’ve designed this daily menopause pack to help restore energy during the day and improve sleep at night.
This is a good time to be tracking your symptoms and looking for triggers. Recording what you eat and drink, when you exercise, how often you pee, etc., may help you determine what triggers hot flashes, night sweats, urgency incontinence (that feeling that you’re not going to make it to the bathroom on time), poor sleep, and more.
You also want to start building your team. This can include a menopause-specialist OB/GYN, a pelvic Physical Therapist, a Health Coach, and your support squad of friends, family, and community. Sound crowded? It doesn’t have to be. Since estrogen decline affects you head-to-toe, shouldn’t your team cover you head-to-toe?
Finally, don’t panic. This phase can be challenging, but there are treatments to help you get through it, healthy and well. Find good, trustworthy (physician-vetted, if possible) information to understand the changes and know what to expect. Consider sharing information with your family and friends, so they can be better supports for you. And definitely consider sharing with younger women, so they have the knowledge they need, right from the start.
This can be a healthy, even wonderful, time of life. Seek help when you need it; it’s here for you.