While we’re used to observing American Heart Month in February, we’re pretty sure we don’t have to tell you about the importance of staying on top of heart health all year round. Our hearts beat all day every day, and we’d like to keep it that way as long as we can.
The statistics about women and heart disease are sobering—even more so when you consider that cardiovascular disease risks increase significantly after menopause due to estrogen’s cardio-protective effect declining as hormone levels decrease during the menopause transition. Lack of information about these risks, combined with the fact that many symptoms of heart conditions can present differently in women than in men, means women often delay seeking and receiving lifesaving care.
While we’d love to wave a magic wand and close that cardiovascular care gap in an instant, healthcare doesn’t work like that. What we can do is educate and encourage women to take an active role (literally!) in supporting their cardiovascular systems for long-term health. One tried and true way to do that? Get moving.
What’s so unique about our bodies at this time that affects our cardiovascular health so much?
To understand why women’s cardiovascular disease risks go up after menopause, we’ve got to turn to that powerhouse hormone, estrogen. Estrogen is believed to have a protective, anti-inflammatory effect on the heart and blood vessels, keeping them flexible for improved blood flow and mitigating the accumulation of plaques that can build up in the arteries (a major contributor to some types of heart disease). Estrogen also helps manage the metabolic processes that keep markers like cholesterol and blood glucose levels in check.
During the decline of estrogen that accompanies menopause, those protective effects decline too, which is why some women see unwelcome changes to their blood pressure, cholesterol levels, and insulin regulation. All of these markers can affect heart and blood vessel health if they get out of control and aren’t managed over time. To make matters worse, the uncomfortable symptoms of hormone swings—like night sweats, hot flashes, and sleep disturbances—may put additional stress on the cardiovascular system by increasing blood pressure and heart rate.
Even circumstances from before menopause can affect our hearts; women who have been pregnant should be aware that a history of pre-eclampsia and gestational diabetes can significantly raise the risk of developing cardiovascular diseases with age.
Is reading all this making you want to get up and do a quick circuit of jumping jacks, squat jumps, and mountain climbers like right now? Honestly, same. Let’s do a few, then dig into some common questions about exercising for heart health before and after menopause.
How does exercise support the cardiovascular system during and after menopause?
We spoke with Stasi Kasianchuk, Gennev’s Senior Director of Lifestyle Care, Registered Dietitian Nutritionist, and certified Exercise Physiologist. She explained what we all need to know about how women can approach heart-healthy exercise from perimenopause through postmenopause.
Exercise can’t bring your estrogen back once it has started to decrease, but it can help your body handle the consequences of this hormonal taper and stay healthier through the natural effects of aging.
Exercise supports your cardiovascular system by:
- Keeping your heart muscle strong so it can pump blood efficiently
- Reducing excess pressure on blood vessels and keeping them limber, allowing them to expand and contract more easily to regulate blood pressure
- Stimulating hormones that support the body in better management of inflammation, which helps prevent damage to blood vessel walls that makes them more susceptible to plaque buildup
- Stimulating the metabolic systems that help your body more efficiently use cholesterol, lipids (the fat in your blood), and glucose for energy, in turn making them less likely to be stored in the body as fat or build up in the bloodstream and form plaque
All the above is true for people of any age, of course, but when you consider how much estrogen does to help these physiological processes work smoothly before menopause, it becomes even clearer that exercise is critical for staying healthy after menopause. It mitigates the effects of dwindling estrogen in a big way.
Can you keep doing aerobic cardio workouts after menopause?
Short answer: YES. If you already have a moderate-to-vigorous cardio workout routine of choice, like running, cycling, swimming, cardio-based exercise classes like dance, or interval training, keep it up, says Stasi. The protective benefits of aerobic exercise for your cardiovascular system are tremendous, and can help ease other bothersome menopause symptoms, like stress and poor sleep.
So where did the idea that you have to give up cardio once you hit menopause come from? As with a lot of ideas about menopause, exercise, and health in general, this probably started as a kernel of truth addressing a very specific situation or piece of research and evolved to become a major misconception.
One thing that could be behind this idea is that many women find that the cardio routines they followed in their 20s and 30s don’t feel as effective as they used to, in that they may no longer ward off the weight gain and body composition shifts that accompany perimenopause and menopause. A common recommendation in that case is for women to try strength or resistance training, like lifting weights or bodyweight exercises. These workouts can more actively build muscle mass than cardio exercises on their own, and more muscle means a lot of good things during menopause: improved metabolic functioning, steadier blood sugar regulation, better bone health, and for some, an easier time managing weight changes. But that’s not to say that they are better than cardio workouts or should replace them altogether.
If you’re still enjoying your cardio routines but feel like you’re working harder than you used to (or would expect to), or struggling to recover as quickly as you’d like, that’s not necessarily a reason to give them up. But you may want to investigate whether perimenopause or menopause could be contributing to your experiences. Your body’s needs for fuel and rest do change with menopause, and it’s normal to feel those effects, especially as age and hormones do their thing and you begin to lose some of the protective effects of estrogen on your arteries, muscles, and bones. It is completely okay to switch up the kind of cardio you do if high-impact aerobic workouts aren’t working for you after menopause.
If you have any concerns about your heart health, talk to your doctor and familiarize yourself with signs of heart disease in women. Stasi also recommends seeking guidance from a credentialed exercise professional and approval from a physician before starting an intense new cardio workout routine.
Is strength training alone enough for cardiovascular health?
Make no mistake: strength training, especially weightlifting, is great for your heart. If you have done resistance training at a level that was at least somewhat challenging, you probably recall breathing faster and feeling your heart beating faster. That is a sign that your heart is pumping harder—nice work! While resistance exercises may not get the heart pumping as vigorously as a high-intensity aerobic workout can, any intentional increase in heart rate is a win. Additionally, by helping you build muscle mass and improve your metabolism, strength training can lower blood pressure, improve blood sugar levels, and improve total cholesterol markers. This is particularly important for preventing the buildup of plaque in the arteries that can decrease blood flow to the heart or brain and cause heart attacks or strokes.
Now, here’s where the devil is in the details. While it is possible to obtain all necessary cardiovascular benefits from weightlifting alone, that usually requires following an intentional and strategic plan created with an exercise professional. Stasi advises that in order to optimally support heart health, most people would benefit from including cardio-specific exercise in addition to weight training.
HIIT workouts: pros and cons of high-impact exercises during menopause and how to do them safely
One encouraging thing about finding workouts for menopause heart health is the range of activities to choose from. Not a runner? Try rowing. Rather be in the water instead of skimming along on top of it? Swimming is great for your heart and easy on your joints if you are one of the “lucky” ones experiencing joint pain. Firmly a creature of dry land? Hiking, especially done at a moderate pace with a few hills in the mix, is a great way to get a dose of cardio plus the added health benefits of spending time in nature.
You get the idea—there are a lot of ways to move, and they can all serve your body a little differently.
Some forms of cardio are considered “low-impact steady state” or LISS, and usually involve keeping the heart rate within a certain beats-per-minute zone for a longer period of time, without a great deal of variation. Other forms fall into a category that might be familiar to you: “high-intensity interval training” or HIIT. HIIT exercises are exactly what they sound like: bursts of intense effort at a fairly high heart rate followed by short rest periods, then repeated. The workouts tend to be short and spicy, with some studies showing they can accelerate fat burning, improve heart rate variability more quickly than moderate steady state cardio, and improve overall cardiometabolic health markers in women.
There’s no question HIIT exercises work your heart, but it’s fair to be curious about whether they’re appropriate during midlife, especially since there’s not a great deal of research about HIIT’s effectiveness for women going through menopause. The intensity can be taxing on your body and some HIIT workouts may involve movements (or accessories, like weights) that take practice to perform at speed without risking injury. Paired with conditions that can come along with aging and/or menopause, like decreased muscle mass and bone density, poor sleep, thyroid disorders, joint issues, high blood pressure, or existing heart disease, HIIT might not be a suitable type of cardio for everyone, particularly those new to exercise or picking it up again after a long break.
If you’re regularly going to HIIT classes, working out without getting injured or experiencing extreme fatigue, adequately fueling and recovering, and feeling pretty good, don’t let us discourage you from your workout of choice! And don’t be afraid to modify your workouts if you need a change; there are many activities you can do in a HIIT format, and you can experiment with different interval lengths to adjust the intensity of your routine.
How to start new heart-healthy exercise routines and move more
If you’re not in the habit of regular cardio exercise, the Physical Activity Guidelines for Americans’ recommendation (supported by the American Heart Association) of 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week, plus at least 2 days of strength training, can sound incredibly daunting. Then again, so does heart disease! Even small changes to get more movement into your routine can have positive effects on your heart health, and building momentum once you’ve gotten started is sometimes easier than taking the first steps.
Our advice?
Start with what feels manageable. Don’t write off walking and lower-impact activities if you’re easing into an exercise routine—just focus on moving more at first. That can even include gardening and yard work, so if you’re not sure what kind of workouts you’d like to try yet, you can work toward meeting your weekly movement goal by raking leaves, mowing the lawn, or briskly weeding the flowerbeds.
Pause to appreciate the movement you do get and what it’s doing for you. Next time the elevator’s out at work and you have to take the stairs with a messenger bag in one hand and a full 64 oz water bottle in the other (cause you’re hydrating your way through menopause like a pro), take a second to appreciate it as, say, cardio in the wild. Reflecting on the positive effects of your daily activities can make you want to look for even more opportunities to move, and it’s nice to remember that you don’t always need to suit up in workout gear to get your heart rate up and work those large muscle groups.
Lean on your team, whether that’s friends who are willing to try a new workout class with you, a doctor or Registered Dietitian Nutritionist who can give you tailored fitness and nutritional advice for menopause, or family members cheering you on for the changes you’re making.
Have more snacks—exercise snacks. “Exercise snacks,” short bursts of heart-pumping activity, aren’t a particularly new concept, but they’re one more way to boost your baseline activity level even on days when you don’t have the time or energy for a workout. There’s plenty of research linking prolonged, uninterrupted periods of sitting to increased risks of heart disease and Type 2 diabetes, but there are things you can do to counteract the effects of sitting too much (even with a desk job!). You might rally a coworker to join you for a walking meeting, or set a timer to remind yourself to get up and move every hour. If you work from home or have a lighthearted workplace, make it fun—a dance break in the kitchen while you heat up your lunch gets the blood moving and is great for morale. The point is not to obsess about how active you are, but to find little ways to break up sedentary periods throughout your day.
Know what motivates you. You don’t have to be an athlete or absolutely love to exercise, but finding your core motivation can go a long way toward making it a regular part of your life. Maybe you’re a data-driven person who likes to track progress over time, or you thrive on routine. Maybe you enjoy setting and reaching goals or are inspired by learning the science behind what exercise does for your body. Maybe you’re feeling feisty and want to live long enough to see true healthcare parity for women—pretty good reason to exercise, if you ask us.
If you’re ready to find your reason, book an appointment with one of our Registered Dietitian Nutritionists for personalized, evidence-based guidance about maintaining a heart-healthy lifestyle through menopause.
Something you should know about Gennev is that we’re not afraid to go there. We’ve covered topics many people are tempted to talk about in whispers, if they talk about them at all: Vaginal atrophy. Lichen sclerosus. Ovarian cysts. Inverted nipples. You may never have thought to search for those phrases, and you may never want to, but if you ever need to, you deserve evidence-based, expert-backed information. Women’s healthcare has long been under-researched, under-served, and under-funded (you could even say it’s under siege…), but that’s all the more reason to have a trustworthy source of accurate answers to your most important questions. This is no time to be coy about our health.
Today, we’re going there to unpack a topic with a lot of chatter around it: the skyrocketing popularity of GLP-1 drugs, a class of medications gaining attention for their use in treating obesity and diabetes.
These drugs are no secret, and weight is not a shameful topic, but we want to acknowledge that not everyone wants to read about weight-related matters for a range of totally valid reasons. If this is not the post for you, that’s okay.
At Gennev, we believe that healthy bodies come in all shapes and sizes, and that if weight management is something you’re interested in, it should be one part of a comprehensive plan to have the kind of healthy life you want, regardless of your age, where you are in menopause, and what’s going on in your world.
That said, we live in a culture that talks a lot about weight: how to lose it, how to keep it off, how to manage it safely and sustainably, why we gain it back. The messaging is hard to miss, and during menopause, it seems to get even louder, as women wonder what’s behind the mysterious “meno belly“ and try to figure out why they seem to gain weight overnight. It’s no wonder, then, that weight loss drugs with a high success rate are getting so much airtime in the cultural conversation.
Since so many are curious about GLP-1s, and Gennev MDs can prescribe them in appropriate circumstances as part of our weight management program, we want you to have all the information you need about this potential option in your menopause weight management toolkit.
But first, some science.
How GLP-1 drugs work
Let’s make the proper introductions: this drug class is broadly known as Glucagon-like Peptide-1 Receptor Agonists. You may know them by their generic pharmaceutical names, like semaglutide, or their commercial brand names like Ozempic or Wegovy (FYI: both Ozempic and Wegovy are brand names for semaglutide, but the drugs are approved and formulated to treat different conditions, so they get different names. The more you know!).
In the body, these medications mimic GLP-1, a naturally occurring hormone that helps manage blood sugar and regulate the appetite. When you eat, the small intestine secretes GLP-1, which signals to other cells that it’s time to perform several digestive and metabolic functions.
The signals that GLP-1 puts out can:
- Help the body process glucose by increasing insulin and blocking glucagon
- Slow gastric emptying (AKA how quickly the food being digested leaves the stomach and releases glucose into the bloodstream) to help you feel full
- Turn on “satiety neurons” in the brain, which balance the hunger and fullness signals that help determine your appetite (and can lead to cravings and “food noise” when imbalanced)
And what about “receptor agonists”? If that sounds like a job title for a secret agent in a spy movie, well, they do kind of act like undercover operators when the body’s systems aren’t working as they should be.
An agonist is a manufactured substance (in this case, synthetic GLP-1 molecules) that binds to a compatible receptor site in or on the surface of a cell. This triggers the effects of the naturally occurring substance (the GLP-1 hormone the body should produce) and tells that cell what to do next (carry out the digestive and metabolic processes the body may struggle to perform on its own).
GLP-1 Receptor Agonists, or just GLP-1s, as you may see them called, have been approved for the treatment of Type 2 diabetes to help regulate blood sugar since 2005. Researchers took notice when patients taking GLP-1s for diabetes also experienced significant weight loss, and in 2014, the FDA approved the first GLP-1 to treat obesity.
Since then, multiple GLP-1 drugs approved for obesity and diabetes treatment have hit the market, with more in development. They also show some promise for treating or lowering the risk of other conditions; while much more data is needed, it’s unsurprising that the drugs have become such a hot topic given all their potential applications.
Criteria for using GLP-1 drugs
Before we go much further, let’s get specific about some terms. With full acknowledgement that GLP-1s are casually called “weight loss drugs” in headline after headline, we’ll mostly refer to “obesity” and “weight management,” rather than “weight loss” in the rest of this article. It’s important to anchor the conversation around GLP-1s on the fact that they’re indicated for something specific: Managing weight concerns, like obesity, associated with metabolic dysfunction and chronic disease”not the normal, gradual weight gain associated with aging (and yes, sometimes menopause).
Gennev’s Chief Medical Officer, Dr. Rebecca Dunsmoor-Su, says this is an important distinction.
“GLP-1s are for obesity, not menopause weight gain. In general insurance companies will not cover these medications for those with a BMI of less than 30, or 27 if they have medical comorbidities related to obesity [like diabetes or heart disease]. We tend to follow these guidelines, as the medications are very expensive if not covered.”
As effective as they are, she says, GLP-1s are not a quick fix, and they’re not for people who need or want to lose the 10-15 pounds that can accompany the transition into midlife (for those folks, Gennev’s menopause-trained MDs and RDNs have many weight management strategies that can be tailored to patient goals). GLP-1s do come with some risks, and can be expensive, subject to shortages, or not covered by insurance, so it’s wise to make an informed decision about whether they’re the right choice before starting them.
That said, there’s always nuance to consider. We know that the hormonal havoc of menopause can raise the risk of metabolic syndrome emerging in those who are genetically predisposed to conditions like high cholesterol, insulin resistance, high blood pressure, and obesity. Sometimes, it does make sense to consider GLP-1 drugs for menopausal patients dealing with metabolic dysfunction identified via lab work.
What to know about taking a GLP-1 for weight management
In an upcoming paper, Gennev physicians Dr. Hana Mikdachi and Dr. Rebecca Dunsmoor-Su note that as popular as GLP-1 drugs have become, they haven’t specifically been studied in peri- or post-menopausal women. This is a major opportunity for further study for a few reasons: many women report that weight gain during menopause feels harder to manage and less responsive to their usual eating and exercise habits, and some anecdotally cite GLP-1s as the most effective intervention they’ve tried.
Also, women in midlife may have other health concerns alongside weight, such as bone health, cardiovascular health, and loss of muscle, which could affect how they respond to GLP-1s. More research on the use of GLP-1s for weight loss during menopause will help both patients and providers understand what kinds of risks and benefits to expect.
The decision to start a GLP-1 should be made with your doctor, who should take a thorough medical history and current health status, including your weight, metabolic profile (for example, cholesterol and blood glucose levels), and consider additional health conditions like heart disease, Type 2 diabetes, or even pre-diabetes”the drugs’ effectiveness at regulating blood sugar levels can help lower the risk of developing more severe metabolic disease.
Dr. Dunsmoor-Su says that patients who come in with questions about the drugs usually want to know about the risks and side effects, and whether they can use them for a short period of time, or if they’re a lifelong commitment.
We’ll break it all down below.
Risks & side effects of GLP-1s
Most GLP-1 medications are administered via injection with a small dosing pen that patients can learn to use at home. As with any drug, GLP-1 side effects can range from mild to severe, and will vary from patient to patient.
More common side effects:
- Gastrointestinal upset like nausea, vomiting, diarrhea, or constipation”these side effects are common and usually resolve as your body adjusts to the medication.
- Injection site skin irritation, itching, or swelling.
Severe but less common side effects:
- Pancreatitis”large-scale studies haven’t consistently shown an increased risk of this side effect, but it may be something to consider if you’ve dealt with pancreatitis or gallstones before.
- Thyroid concerns”some animal studies have linked GLP-1s to thyroid cancers, though this doesn’t suggest an increased risk in humans. Data doesn’t show strong evidence for the connection, but it’s something researchers will continue to study.
- Gastroparesis”one expected function of GLP-1s is to slow gastric emptying. Some people experience an extreme version of this in which stomach muscles move food too slowly, causing abdominal discomfort and trouble with digestion.
Who shouldn’t take GLP-1s?
The FDA recommends that patients with certain conditions avoid GLP-1s. Some of these contraindications are due to known serious risks, and others are out of an abundance of caution based on early or inconclusive studies.
These conditions include:
- Medullary thyroid cancer or a family history of the disease
- Multiple endocrine neoplasia, a group of disorders that cause tumors on hormone-producing glands in the endocrine system
- Pregnancy, due to potential risk for birth defects”so if you’re perimenopausal, take note! Even irregular periods mean you could still get pregnant, so please talk to your doctor if you’re considering GLP-1s during perimenopause.
“Do people have to stay on GLP-1 drugs forever?
The answer to this is quite complicated and may depend on the patient and why they’re taking the drug. The medical community is still learning about the long-term outcomes of GLP-1 usage for weight management, and what happens when the drugs are discontinued.
Here’s what we do know:
- Lifestyle adjustments alongside GLP-1 use are important no matter what dosage is being taken or for how long. A healthy diet and physical activity are essential complements to GLP-1 use, and maintaining these habits can help patients get to a healthy weight.
- Discontinuing GLP-1 use can result in rebound weight gain. When a GLP-1 no longer influences metabolic, digestive, and neurologic processes, dysfunctions like poor blood sugar regulation and abnormal appetite cues from the brain can start up again, which can lead to the patient regaining weight. The important takeaway here is that these drugs help manage the metabolic conditions that contribute to weight gain, but do not permanently cure them.
- Some researchers suspect that reducing GLP-1 medication dosage through a slow, sustained taper (instead of rapidly decreasing dosage over a short period of time, or stopping them suddenly altogether), could help some patients prevent rebound weight gain, but we’ll need more data to confirm this with any confidence or say why it might be the case. Several studies are underway to determine whether this would be an effective method for patients who wish to stop using GLP-1s but still maintain their weight.
Compounded semaglutide: Why we don’t recommend it
We promised you real talk, so let’s touch on another important topic in the GLP-1 conversation: compounded drugs.
Compounded drugs are not generic versions of brand-name formulas, but custom-made compounds assembled in pharmacies or independent labs. They’re sometimes used when a patient can’t tolerate an ingredient in a generic or branded drug, and are often cheaper to purchase and not subject to ingredient shortages that can make drugs harder or more expensive to make.
The catch? Compounded drugs aren’t FDA-approved, and the standards of the facilities that produce them vary widely. This makes it virtually impossible to guarantee the safety, effectiveness, quality, or dosage accuracy of compounded formulas and the ingredients used to create them.
Compounded semaglutide for weight loss can look like an appealing option to those starting to explore the GLP-1 landscape. It’s custom-made, may be more widely available and more affordable than prescription medications like Wegovy, particularly when insurance won’t cover them, and comes tidily marketed by direct-to-consumer companies with slick branding. Some companies even make it easy to buy compounded semaglutide online without an in-depth conversation with a doctor”sounds fast and simple, but this can be dangerous.
Another thing to watch for is murky labeling issues, since some companies describe their compounded GLP-1 formulas as “generics.” This is misleading, since generic drug formulas are FDA-regulated and must meet the same ingredient, safety, dosing, manufacturing, and quality standards as their brand-name counterparts. As of February 2025, when we’re writing this, there is no approved generic formula for any GLP-1 drug”anywhere. What this means is that any medication being marketed as “generic” semaglutide is, in fact, a compounded drug using unregulated imported ingredients. That’s a significant ethical and health concern, since there’s no easy way to know what these ingredients are, how much of them the formula actually contains, or what risks they present to patients.
We don’t want to scare or shame anyone for being curious about compounded semaglutide or other compounded GLP-1 drugs, but the unfortunate truth is that these formulas can come with serious safety concerns, so we at Gennev do not prescribe or recommend them. The FDA issued a statement in December 2024 about the risk of using unapproved GLP-1 formulas, and all North American obesity medicine societies recommend against their use as well.
Gennev’s approach to menopause weight management
It’s an incredible time to be in women’s healthcare, breaking taboos and giving women the information they need to make responsible decisions about their well-being. We know everyone has a unique relationship to the topic of weight, shaped by decades (okay, an eternity) of cultural conditioning and personal experiences, but that’s why we speak candidly about it”particularly during times like menopause, when our bodies start pulling stunts we’ve never seen before and it’s hard to know what advice to trust.
We’ve created a patient-focused, evidence-based weight management program (eligible for self-referral under some insurance providers) meant for exactly that situation: your body’s changing, you’re not sure how to feel about it, and you want to protect your long-term health. GLP-1 medications may or may not ultimately be part of your strategy, but the good news is you’ll have plenty of ways to reach and stay at a healthy weight, overseen by our menopause-trained Registered Dietitian Nutritionists and MDs.
Dr. Dunsmoor-Su sums it up: “We designed the program to focus first and foremost on lifestyle changes and the support to make those [by] working with an RDN. These are the changes that will over the long term make the most difference. When thinking about medications (GLP-1 or others) we consider other medical conditions, other symptoms and what medication interactions might be an issue. Even if GLP-1 medications are inaccessible due to cost there are other medications that might help, and we can discuss risks and benefits of these.”
So if menopausal weight gain is on your mind, and the chatter about semaglutide and other GLP-1 medications has you curious, please don’t be shy. We hope we’ve given you plenty of information to consider about these drugs and the variety of options for healthy, body-positive weight management through Gennev. If you have more questions or are ready to try something new, book your intake to get started.
Real quick—off the top of your head, can you name everything you’ve done today? If you’re reading this over your morning coffee, your list might be short: woke up, walked the dog, made breakfast, and sat down to catch up on Gennev’s blog. If you’re reading this on your commute home from work, it’s fair to say your list might be a little longer. No matter what’s on it, we’re going to guess there are a few things it probably doesn’t include:
- Breathe in, breathe out (repeat 22,000 times)
- Circulate blood to brain
- Make new skin cells to heal that cut you got shaving
- Convert this morning’s egg on toast to lipids, glucose, and amino acids
- Increase shivering rate for the office’s arctic temperatures (pause for hot flash)…
And thank goodness, right? If we had to add biochemical bodily functions to our to-do lists on top of everything else we juggle, we just might lose it. Luckily, we all come with built-in programming that handles many of those processes for us without any extra planning on our part: our metabolism.
The lowdown on metabolism during menopause
Wait, how does the metabolism work again?
Think of the metabolism as a sort of engine that runs two complementary processes:
Catabolism, in which your body breaks down nutrients to create energy (a process that includes burning calories)
and
Anabolism, which uses that energy to build and repair molecules in the body. These can go on to become new or healed tissue (for example, muscle growth after exercise).
When these processes are in sync, your body can do everything it needs to: breathe, digest food, circulate blood, regulate hormones, eliminate waste—all the things you’re glad to not have to put on your daily to-do list, because if all’s going well inside, they’re already getting done.
What’s going on with my metabolism during menopause?
To understand what can happen to your metabolism during menopause, it’s helpful to frame overall metabolic health as “the balance of nutrients and activity that supports the fundamental systems that run your body,” says Gennev’s Chief Medical Officer Dr. Rebecca Dunsmoor-Su. She emphasizes that metabolic health is highly variable between individuals and depends a great deal on genetics, lifestyle, and personal risk factors. Supporting a healthy metabolism at any age requires understanding and balancing your body’s needs for fuel, movement, and rest.
Midlife ushers in unique circumstances for women, though. As we age, especially during the transition into menopause, the balance between those needs for energy, activity, and recovery starts to shift, and the body reacts accordingly. Dr. Dunsmoor-Su reminds her patients that this is not unusual. She explains that if you’ve noticed changes to your energy levels, appetite, body composition (i.e., where you carry your weight), or bloodwork (like cholesterol and blood sugar levels), you’re not imagining them; they can be a normal part of aging, to an extent, and a consequence of hormonal fluctuations starting even in perimenopause. (Fun, we know.)
If it feels like your menopausal body has a whole new set of demands lately, Dr. Dunsmoor-Su confirms that may not be far from the truth. Reacting to your body’s changing needs is key for staying metabolically healthy, she says, and maintaining that nutrient-activity balance after menopause can require different proportions of nutrients, different types of exercise, and more attention to quality rest for optimal health.
This is by no means impossible, particularly if you’re not genetically predisposed to certain metabolic disorders (we’ll get to those), but you may already know that it can take a little extra patience, creativity, and support to make the lifestyle changes that will keep your metabolism thriving.
If patience and creativity alone aren’t getting you where you want to be on your menopause journey, let Gennev add the support. Make an appointment with a menopause-trained MD or RDN today.
Understanding metabolic syndrome during menopause
If some changes are normal, what kinds of metabolic changes during menopause should I be concerned about?
While everyone can expect some metabolic changes as they age, some people may be prone to metabolic disorders that can arise or worsen during menopause due to genetic and lifestyle factors. One example is a term you may have heard before: metabolic syndrome.
Metabolic syndrome describes a cluster of disorders, most related to your body’s ability to process insulin, that can raise the risk of Type 2 diabetes, stroke, and cardiovascular disease. It’s commonly indicated by having three or more of the following biomarkers, which are considered out of range for optimal metabolic health:
- Fasting blood glucose above 100 mg/dL
- HDL cholesterol less than 50 mg/dL for women
- Triglycerides above 150 mg/dL
- A waistline of 35 inches or greater for women
- High blood pressure (130/85 or higher)
For those genetically predisposed to metabolic syndrome, menopause may be the time when these conditions begin to show up, affect your health, and become more challenging to treat.
Menopause strikes again. Why does this happen?
There’s a lot we’re still learning, but from a physiological standpoint, some conditions that contribute to metabolic syndrome during menopause can be due to hormonal changes. Hormones like estrogen, progesterone, testosterone, and insulin are just a few of the key players in the metabolic processes that your body needs to function. When their levels fluctuate during perimenopause and menopause, it can lead to a cascade of consequences that can include:
- Increased insulin resistance and difficulty removing glucose from the bloodstream to regulate blood sugar
- Changes in sleep habits which impact appetite and energy levels
- Changes in bone density, muscle mass, and body fat quantity, type, and distribution
- Increased inflammation in multiple organ systems, including the cardiovascular system
These changes also often come along just as midlife throws its curveballs: you hit a career high with a big promotion, but it leaves less time to fix healthy home-packed lunches. Your kids and aging parents are somehow both keeping you up at night. Staying active has gotten harder as your family’s schedule has gotten busier. You have global news, celebrity gossip, and life updates from everyone you know at your fingertips 24/7. And you’re supposed to be able to clear your mind and de-stress just like that?!
Between the onslaught of hormonal changes, physical symptoms, and lifestyle stressors that can make those symptoms tougher to manage, it’s no surprise that menopause is the time when disorders like metabolic syndrome may start to come out in full force. This is concerning because without intervention, conditions like insulin resistance and inflammation can get worse. These in turn can raise the risk of cardiovascular disease, stroke, diabetes, thyroid disease, and even cancer—all good reasons to take metabolic syndrome seriously.
Staying metabolically healthy during menopause
It’s important to keep in mind that menopause doesn’t automatically come with a side of metabolic syndrome despite the increased risks due to hormone changes, and there are steps you can take to start improving your health and metabolic function at any time. This is true during perimenopause too, when many women first notice body composition changes or get unexpected results from lab work—sometimes the first signs that metabolic shifts might be taking place.
It can be disconcerting when these changes and symptoms come along, so we always encourage women to seek support from providers who are knowledgeable about menopause.
If you have specific concerns, or want some guidance about what to prioritize, chat with a doctor or Registered Dietitian Nutritionist. They’ll help you make a plan that might include diet, regular exercise, and lifestyle changes to reach your desired goals. Your doctor may also discuss hormone therapy and medication, if appropriate, and both providers can discuss the impacts of the various treatments that may be available to you.
Gennev clinicians in action
Helping patients find long-term solutions for their unique health concerns during menopause requires thoughtful detective work from Gennev MDs and RDNs. Like other Gennev clinicians, Melissa Burton, RDN, looks well beyond standard lab work to take a holistic look at all factors that could be contributing to her patients’ symptoms.
Though Gennev RDNs don’t order lab work, they work closely with MDs and patients to get all the necessary information for a thorough intake. When Melissa begins working with a new patient, for example, she may recommend they have their doctor order labs like a complete cholesterol panel, which measures LDL cholesterol levels alongside HDL and triglycerides, and tests that measure glycemic control over a period of months instead of hours, which may give her more information than a single fasting blood glucose test.
She’ll consider vitamin and nutrient deficiencies; low levels of Vitamin D, Vitamin B12, and iron—to name a few—are common culprits of many symptoms that can crop up during midlife. She’ll also ask her patients about stress, sleep, and other lifestyle factors, and have them keep a thorough food journal to keep track of what they eat and when. All these details help Melissa get a complete picture of what may be going on for her patients metabolically, so she can craft a plan to help them manage their symptoms and health conditions.
Dr. Dunsmoor-Su adds that Gennev patients can talk with an MD about their risk for diabetes and cardiovascular disease, particularly if there’s a family history of those conditions to consider. She also encourages patients to explore whether hormone therapy could play a role in reducing certain troublesome symptoms during menopause and the long-term health risks associated with them.
I’m ready to support my menopausal metabolic health. Where do I start?
Feeling motivated? You don’t have to figure it out alone. Check out our tips for the best exercises for metabolic health, read up on dietary tips for hormonal weight gain from Gennev’s Registered Dietitian Nutritionists, or incorporate more delicious anti-inflammatory foods for a simple change you can make right away.
Your metabolic health wasn’t determined in a single day, though sometimes it can feel like menopause wreaked havoc on it overnight. Whatever you’re going through, even small adjustments are worth it for your long-term well-being. If you’re eager to learn more about how to keep your metabolism healthy during menopause, reach out to a Gennev menopause specialist to get started with a personalized care plan.
The holiday season is a time of giving, and finding the perfect gift for the women in your life can be a meaningful way to show you care. For women experiencing menopause, a thoughtful gift can go beyond the ordinary, offering comfort, empowerment, and a reminder that their wellness matters. Whether you’re shopping for your mother, sister, friend, or partner, gifts that support her journey through menopause can make this season even more special.
From cozy solutions for those sleepless nights to self-care essentials that celebrate her strength and resilience, this guide is full of holiday-inspired gift ideas that she’s sure to appreciate.
Self-Care Essentials: Pamper and Relax
Menopause often brings stress and fatigue, making self-care gifts a practical choice. Consider:
- “Aromatherapy Diffusers and Essential Oils: Scents like lavender and chamomile can promote relaxation and improve sleep quality.“
- Spa Kits: Sets that include body scrubs, bath salts, and soothing lotions can provide a calming experience.“
- Weighted Blankets: These can offer comfort and help improve sleep, which is often disrupted during menopause.“
- Luxurious Robes or Pajamas: Opt for breathable fabrics like bamboo or cotton to help manage hot flashes.
Wellness Tools:Health Meets Comfort
Well-being is crucial during menopause. Support her health with these practical gifts:
- “Cooling Pillows and Bed Sheets: Designed to combat night sweats, these can make bedtime more comfortable.“
- Reusable Cooling Towels: Ideal for on-the-go relief from hot flashes.“
- Herbal Teas: Blends with ingredients like black cohosh or chamomile can help balance hormones and soothe nerves.“
- Menopause Supplements: High-quality vitamins and minerals that support hormone health (consult a healthcare professional before gifting).“
- A Gennev Appointment: Give the gift of expert care with a consultation tailored specifically to her menopause journey.This provides access to medical advice, symptom management, and personalized wellness strategies from professionals who truly understand.
Gifts That Encourage Movement and Fitness
Staying active is crucial during menopause for managing weight, boosting mood, and maintaining bone health. Consider these fitness-focused gift ideas:
- “Yoga Mats and Accessories: A non-slip mat, yoga blocks, and straps are ideal for beginners and experienced yogis alike.“
- Free Weights: A set of 2 lbs, 5 lbs, and10 lbs weights can support strength training, an essential activity for bone health and muscle maintenance.“
- Walking Shoes: High-quality, supportive footwear that ensures comfort and enjoyment during daily walks.“
- Fitness Tracker: Monitors steps, sleep,and activity levels to encourage a healthy lifestyle.“
- Online Fitness Subscriptions: Tailored programs for women over 40 to inspire and motivate consistent movement.
Mind and Soul Nourishment
Menopause is as much a mental journey as a physical one. Help her stay positive and mindful with these ideas:
- “Journals and Guided Planners: Writing can be a therapeutic outlet for emotions.“
- Inspirational Books: Titles about empowerment, wellness, or the menopause journey can be uplifting.“
- Meditation Apps or Subscriptions: Consider apps like Calm or Headspace for guided relaxation sessions.“
- Craft Kits: Knitting, painting, or pottery sets can be a fun and creative distraction.
Fashion for Function and Style
Clothing that prioritizes comfort without sacrificing style is a winner:
- “Breathable Layers: Cardigans, wraps, and lightweight scarves are both stylish and practical for temperature fluctuations.“
- Moisture-Wicking Activewear: Great for workouts or casual wear, these fabrics keep her cool and comfortable.“
- Supportive Undergarments: Seamless, comfortable bras and panties designed for sensitive skin can be a thoughtful gift.
Tech Gifts
Modern problems call for modern solutions. Tech gifts can help manage symptoms:
- “Smart Fans: Small, portable, and adjustable fans for desk or bedside use.“
- Red Light Therapy Devices: Known for promoting skin health and reducing inflammation.“
- Temperature-Controlled Mugs: Keep beverages warm for longer, ideal for cozy tea moments.“
- Blue Light Glasses: Help alleviate screen strain, especially if she experiences headaches or insomnia.
Personalized and Sentimental Gifts
Sometimes, the most meaningful gifts are those tailored to her unique preferences:
- “Customized Jewelry: A bracelet or necklace engraved with a motivational quote or personal message.“
- Photo Books: Highlight cherished memories with family and friends.“
- Subscription Boxes: Curated wellness, skincare, or self-care boxes delivered monthly can be a delightful treat.“
- Handwritten Letters: Share your appreciation and admiration for her journey”it’s a heartfelt gesture money can’t buy.
Culinary Gifts
Nourishment and comfort often go hand-in-hand:“
- “Healthy Cookbooks: Focused on hormone-balancing meals or anti-inflammatory diets.“
- High-Quality Herbal Blends: Include teas or spices known to support hormonal health.“
- Kitchen Gadgets: An air fryer, blender, or soup maker can simplify healthy cooking.
Experiences Over Things
If she values experiences more than material gifts, consider these:
- “Spa Days or Massage Vouchers: A luxurious way to relax and rejuvenate.“
- Weekend Getaways: Plan a serene escape to a calming destination.“
- Cooking or Art Classes: A chance to learn and socialize in a low-stress environment.
Gennev Employee Recommendations
For a truly thoughtful and expert-driven gift, consider these recommendations from the Gennev team.
Books for Inspiration and Empowerment
- “The Balanced Plate: A Simple Formula for Building Nutritious Family Meals by Monika Jacobson “ A guide to creating simple, healthy meals for the whole family.“
- The Menopause Manifesto by Dr. Jen Gunter “ A definitive resource on understanding menopause and embracing this life stage.“
- Come As You Are by Emily Nagoski “ A revolutionary book on women’s sexual health and wellness.“
- A Tired Woman’s Guide to Passionate Sex by Laurie Mintz “ Practical advice for reigniting passion in relationships.“
- All Fours by Miranda July “ An unexpected romp through the anxiety and sexuality of a female protagonist navigating perimenopause.“
- Burnout by Emily Nagoski and Amelia Nagoski “ Insights into breaking free from stress and finding joy.
Health and Comfort Solutions
- Cooling Bra Inserts by Joylux “ Offers relief from hot flashes while ensuring comfort.“
- Chili Pad “ A cooling mattress pad that promotes better sleep by regulating temperature.“
- A Subscription to Rosy Wellness “ Provides [BS3] [HR4] access to resources, tools, and expert guidance for sexual health and overall well-being.
Beauty and Skincare
- “Skincare by Kari Gran “ Luxurious and natural skincare products to soothe and hydrate.
Clothing for Comfort
- “32 Degrees Clothing “ Affordable, high-quality comfort clothing for both summer and winter, perfect for temperature regulation.
Final Thoughts
Menopause is a complex and deeply personal journey. The most meaningful gifts are those that show thoughtfulness, understanding, and love. Whether you choose a wellness item, an experience, or a sentimental keepsake, your gesture will remind her that she’s supported and cherished during this transitional stage. This shopping season, let your gift speak volumes about your care and appreciation. Happy Holidays!
The holiday season is full of joy, connection, and tradition, but it can also bring stress, overwhelm, and sensory overload. Amid the hustle, it’s easy to lose sight of our own needs as we focus on others. This is where interoception”the ability to sense, acknowledge, and interpret bodily signals”becomes a powerful tool for self-care.
What Is Interoception?
Interoception refers to the practice of noticing and understanding the signals your body sends, such as hunger, fullness, satisfaction, thirst, or even tension in your shoulders. It’s a foundational part of Intuitive Eating, a self-care framework created by two dietitians in 1995 that integrates instinct, emotion, and rational thought to help individuals foster a healthier relationship with food.
In Intuitive Eating, interoception helps you connect with your body’s cues to gauge hunger and fullness, and to determine what truly satisfies you. But during the holidays, with their abundance of sensory input”sights, smells, sounds, textures, people, and activities”interoception can extend far beyond eating.
The Holiday Season: A Time to Pause and Tune In
The holiday season is rich with opportunities for sensory and emotional experiences. It’s a time to connect with loved ones, enjoy delicious meals, and reflect on the year. But it’s also a time of heightened busyness, which can make it challenging to care for yourself. Cultivating interoception can help you navigate the season with more intention and balance.
Consider these two levels of interoception:
Macro-Level Awareness
Take a moment to step back and reflect on how the holidays make you feel.
Positive Emotions: What activities, moments, or traditions bring you joy, energy, or peace? Lean into these experiences. Allow them to become part of your personal emotional reservoir”resources you can draw upon when you need a boost.
Negative Emotions: What leaves you feeling sad, anxious, or exhausted? Notice your reactions and instincts. Instead of reacting impulsively, pause to explore strategies that might make these moments less overwhelming.
By labeling your emotions”whether positive or negative”you gain insight into how to approach each situation in a way that aligns with your needs.
Micro-Level Focus
Zoom in on specific experiences, such as food, drink, or activities, and observe how they affect you.
Acknowledge how novelty might influence your reactions: Do you feel the urge to try everything, risking overindulgence? Or do you set strict limits that leave you feeling restricted?
Pause and check in with your body. Notice your breathing, jaw tension, or whether you feel hungry, thirsty, tired, or overwhelmed.
The Pause-Evaluation-Action Cycle
The practice of pausing, reflecting, and choosing your next step can be a game-changer during the holidays.
Pause: Stop and tune into your body. What signals is it sending?
“
Evaluate: Are you content with the current sensation, or do you want to change it?
“
Act: If you want to continue, keep going and set a time to check in again. If you want to make a change, identify the feeling you want to achieve (calm, focus, satisfaction, etc.). Consider what you need to support that change”relaxation, energy, compassion”and take action.
Repeat this cycle throughout the day to navigate moments of hunger, fullness, satisfaction, and even emotional highs and lows with greater clarity and intention.
A Season of Self-Care and Connection
Whether it’s savoring your favorite holiday dish, managing a packed social calendar, or navigating tricky family dynamics, interoception offers a pathway to balance. By noticing and responding to your body’s signals, you can take better care of yourself while sharing the joy of the season with those around you.
This holiday season, let interoception be your guide to both giving and receiving”starting with yourself.
“
Here’s one for the story books, where two twenty-somethings working for a women’s health company DM a Gen X icon and the rest is history.
Gennev’s Director of Performance Marketing and Social Media Manager, Isabella Rusher and Haley Roberts, created a once-in-a-lifetime opportunity to collaborate with the legendary Candace Bushnell. This collaboration has been a dream come true, and we’re thrilled to share the details.
It All Started with an Instagram DM
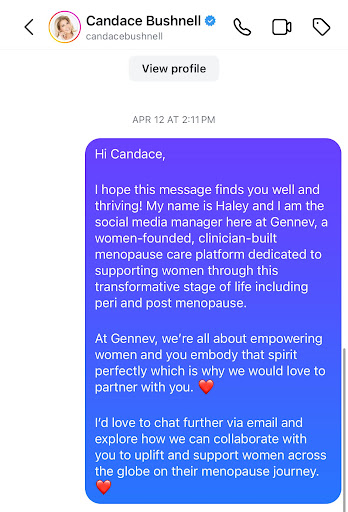
Like so many great connections these days, we reached out to Candace on Instagram after seeing how she talks so openly about women’s health, and specifically menopause. Her candidness and humor resonated with us, and we knew we had nothing to lose. Luckily, she responded. From there, our team quickly set up a Zoom meeting, and that’s when things fell into place.
During that first virtual meeting, it was clear that Candace shared our passion for breaking the silence around menopause and empowering women to embrace this phase of life.She immediately connected with Jill, our founder and CEO, and their shared vision for supporting women in midlife clicked. We all left that call feeling like we were onto something big.
Meeting Candace in Person: A One-Woman Show
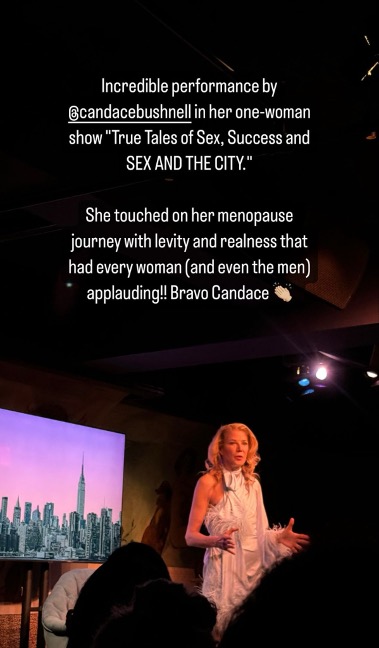
We seized the chance to see Candace live in her one-woman show: True Tales of Sex, Success, and Sex and the City. It was one of the most inspiring performances we have ever seen. Not only was Candace hilarious while sharing her story navigating New York City and becoming a best-selling author, but she used her platform to discuss the experiences of women going through menopause. She approached the subject with confidence, beauty and SEXINESS, words that are often not associated with menopause. We left the show empowered and more passionate than ever to share that feeling with the rest of the world.
The Photoshoot: Bringing It All Together

Next step, bringing the campaign to life. Haley, also a talented photographer, had the honor of photographing Candace. She brought such elegance, style, and fun to the shoot, which made capturing her spirit easy. Isabella was there directing, ensuring that we told the story we wanted: that menopause is a journey women can go through with confidence and grace, and that they don’t have to do it alone with resources available like Gennev, and so many other wonderful menopause care providers.
Working with Candace in person was everything we’d hoped it would be and more. There was such a natural chemistry between everyone on set, and we truly believe that shows in the photos.
Transcending Age Stigmas
For Isabella and Haley, this partnership is especially meaningful because they are 20-something women who, prior to working at Gennev, had little knowledge of menopause and its challenges. They have learned so much about the difficult changes women face in menopause” physically, mentally and emotionally. Candidly, they felt ashamed of their lack of knowledge and ignorance on the topic. They have mothers, grandmothers, aunts and friends who have either gone through menopause, or one day will, and yet they were not equipped with the education or resources to help. With this campaign, we hope to transcend generational stigmas and bring women of all ages together for an inevitable phase of life.
Whether you’re in your teens, 20s, 30s, 50s, or beyond, these conversations matter, and we want to make sure they’re happening.
Conversations around women’s health are becoming less taboo, but at Gennev we’re here to show that menopause is something everyone can talk about”not just women in their inner circles.
What’s Next for Gennev x Candace Bushnell
This is just the beginning of what’s to come. We’re working on creating content that’s going to spark important conversations around menopause, featuring expert advice, personal stories, and a community of women supporting each other. Candace’s voice and influence will help us reach women who might not have considered talking about menopause before or felt comfortable enough to seek help for their symptoms. We’re beyond excited to see where this journey takes us and the incredible women we will empower along the way.
“
About ten years ago, I was sitting at a table surrounded by senior women leaders at a tech company where I worked. This was the monthly executive female leader networking dinner that I managed, and I eagerly anticipated rubbing shoulders with experienced and powerful women at the top of their game.
What caught my attention on this particular evening was how a small group was talking about menopause. They were speaking in hushed tones as they talked about lack of sleep, inability to come to work because of extreme periods, and their growing waistlines.
It dawned on me that this community had transitioned from talking about babies, maternity leave and childcare to sharing experiences about a new phase in life. One that was starting to impact their careers and job performance.
Since that moment, there has been a mantra roaming about my head that I just can’t get rid of. How do we change the face of workplace benefits to support women in menopause? Little did I know that I would get to be part of that change years later.
Today, Gennev joins forces with Progyny to bring menopause care to the workplace. This care goes beyond work leave policies, educational sessions, and community forums, to bring menopause-trained OB/GYNs and Registered Dietitian Nutritionists to workplace benefits.
Let me be more clear, this means that specialty menopause care will be covered for employees and their dependents. Gennev and Progyny make it possible for women to effectively advance in their careers and manage their changing health and well-being at the same time.
Why are Menopause Workplace Benefits Important?
If you’re a woman, you’re likely to respond, “”¦because I’m worth it!” In all seriousness, the number one reason for providing employees and their dependents access to menopause-trained OB/GYNs and Registered Dietitians is to improve their quality of life. We know from talking with our patients that 89% experience menopause symptom improvement after working with our clinicians.
I’ve also heard how menopause care improves the ability to perform in their jobs. “Life-changing” and “I got my brain back” are common pieces of feedback. A patient who has been working with a Gennev OB/GYN and a Dietitian for three years recently told us that she “felt like herself again.” You can’t put a number on results like that!
Most importantly, menopause care prevents downstream health concerns commonly triggered during the menopause transition, including cardiovascular disease, osteoporosis, mental health and depression.
In July 2023, Gennev commissioned a study through Milliman on the healthcare costs of menopause, and found that medical and prescription costs for women ages 45-54 with menopausal symptoms are 47% higher compared to women of the same age not experiencing menopause. The expense for these women comes to $1,243 per patient per month compared to $848 per patient per month, respectively.
Now, from the perspective of a business decision maker who needs to manage employee benefits within a budget, here’s a nugget that underscores the case for menopause-covered benefits delivered by Gennev: you will see upwards of 71% cost savings in healthcare cost per person experiencing menopause.
What’s more, according to an April 2023 report from the Mayo Clinic, menopause is costing employers an estimated $1.8 billion in lost work time per year and $26.6 billion annually when medical expenses are added, in the U.S. alone. It’s tough to argue the math when the costs are real.
In a market where women of menopause age comprise 20% of the U.S. workforce and unemployment among women is at an all-time low of 3.4%, employers need women. Not only that, but companies need women in their 40s, 50s, and 60s who are skilled workers and experienced leaders.
Offering targeted menopause benefits can be a strategic advantage for talent acquisition and retention. For current employees, it fosters a supportive and inclusive culture that empowers women to excel professionally. For hiring, particularly given how competitive the labor market is, providing comprehensive support for women in this stage of life can truly set an employer apart.
What Can You Do?
If you’re a working woman”whether you’re of menopause age or not”forward this article to your human resources team. Gennev has seen women rise up on several occasions and advocate for specialty menopause care coverage under their workplace benefits. And it works. We hear from large and small companies who are leaning on their Health Plans to expand coverage for menopause care provided by companies like Gennev. We’ve seen workplace benefits and support for mental health and well-being significantly evolve over the past decade. Why should menopause be any different?
If you’re an employer, examine the costs you may be incurring. When I speak with employers, I commonly ask how much they’re spending on health coverage for employees and dependents in the menopause time of life. Most often, their response is, “I don’t know.”
If you need support diving into the numbers, examining near-term and long-term benefits you can offer for menopause care, you can learn more by reading the Gennev Workplace Benefits Whitepaper. If you would prefer to meet with a Gennev workplace specialist, please email partnerships@gennev.com or call 206.894.4292.
“
Lack of access to quality, specialized medical care for menopause is causing women to suffer needlessly and the U.S. healthcare system to bear the brunt of unnecessary costs.
Gennev commissioned a study through Milliman, one of the world’s largest independent actuarial and consulting firms, to understand the costs of not treating menopause, and how we can help reduce costs and improve health outcomes in menopause.
The study, Healthcare Cost and Utilization for Women in Menopause found that medical and prescription costs for women ages 45-54 experiencing menopause are 47 percent higher on average than the general population of women in the same age band. The per member per month expense for these women experiencing menopause averaged $1,243, compared to $848 for the total population.
Why Are Costs Higher During Menopause?
According to the study, women ages 45-54 exhibiting symptoms of menopause have a 41 percent higher utilization of professional medical services and twice the behavioral health costs than the general population of women in the same age band.
Furthermore, anxiety, a widely reported prevalent symptom of menopause, can be effectively alleviated by treating the root cause of menopause itself.
“The cost of overlooking menopause goes far beyond financial implications. It exacts a heavy toll on women’s overall well-being”physically, emotionally, and financially,” said Dr. Rebecca Dunsmoor-Su, Chief Medical Officer at Gennev.
She goes on to say that “”¦there’s a massive knowledge gap. Our study estimates 80 percent of women between the ages of 45 and 54 could be experiencing menopause symptoms at a given time, yet, based on diagnosis and treatment coded in claims data, only 21 percent seek treatment. This discrepancy underscores the importance of not only recognizing the need for comprehensive menopause care and prioritizing coverage, but the critical need to raise awareness about menopause care. We can empower women to navigate this transformative stage with grace and ensure they receive the support and care they rightfully deserve.”
Does Hormone Replacement Therapy Impact Costs?
The study also highlights how women in the study group using hormone replacement therapy (HRT) have 11 percent lower overall healthcare costs compared to women using other menopause therapies.
Furthermore, treating menopause can yield far-reaching advantages that extend beyond financial savings. Specifically, women in the study group who use HRT during menopause show 14 percent lower health costs associated with substance abuse disorders as compared to general medical utilizers.
How Can a Menopause-Trained Provider Help?
Regardless of chosen treatment path, Gennev knows the impact seeing a medical professional who is trained in menopause can have to a woman going through it. However, quality menopause care isn’t easy to find. According to a John Hopkins-led survey, only one in five OB/GYNs take the menopause seminar in medical school. That number is likely even less for primary care doctors.
Gennev providers have already helped thousands of U.S. women improve their quality of life by prescribing personalized, evidence-based treatment plans and delivering the virtual support needed for those plans to succeed. Integrated treatment plans may include prescription medication, nutrition, fitness, sleep, mindfulness, and behavioral health therapies.
Learn how a menopause-trained provider can help you feel better.
Read The Full Report: https://www.milliman.com/en/insight/healthcare-cost-utilization-women-in-menopause
How this Boeing engineer managed her menopause in the workplace
Born and raised in the macho culture of Venezuela, educated entirely in a conservative Catholic school system, and now often the only woman in the room at Boeing, engineer LL is used to keeping anything related to “women’s stuff” on the down-low, pardon the expression.
But keeping frequent, intense hot flashes to yourself isn’t easy. And when you couple those hot flashes with cancer treatment, keeping it quiet can become a real burden. This is LL’s story of managing her health”and her hot flashes”while keeping her cool.
At age 52, LL hadn’t yet gone through menopause. She’d started having periods late (age 17); now it appeared she’d be delayed on the other end as well.
Then she was diagnosed with breast cancer as
estrogen-positive breast cancer, the kind that grows
faster in the presence of estrogen.
As part of her treatment, the doctor prescribed medication that would stop estrogen production and force menopause. But her body refused to cooperate. It took six years before she had her first hot flash. “The doctor kept asking, “Have you had a hot flash yet?’ And when I said no, not yet, he was frustrated. But it’s not my fault; I am not doing it on purpose!”
When it finally happened, LL, a planner, started figuring out how to handle it in the mostly male environment of Boeing. “But how do you plan for something that can happen any time of the day, any number of times, without warning?” An engineer, she naturally started looking for patterns, but discovered only that her hot flashes last 3 to 5 minutes, which wasn’t a lot of help in figuring out how to avoid “sharing” her experience.
Do you deal with embarrassing, even debilitating hot flashes?
Talk to one of Gennev’s menopause experts via our telemed, and
get the help you need from the comfort of your own home.
“I was raised by French Catholic nuns in Venezuela,” LL says, laughing. “I was taught you have to behave like a queen outside of your house. So my husband and daughter were the only ones who knew what was happening! At home I was throwing off my clothes and bitching about how hot I was.”
“At work? I’m the Queen of France, I’m Marie Antoinette. The Queen of France would not show she has hot flashes.”
Keeping hot flashes under wraps”when being “under wraps” is the last thing she wants”is a challenge.
“I’m so relieved when someone says, “Is it hot in here?’ It’s permission to throw off my jacket”Boeing has these wonderful, cozy, reflective, fleece jackets that we must use because we work in a giant, chilly hangar and transit across risky tarmac. Besides, it is always cold in the Pacific Northwest, so fleece is key! But fleece doesn’t absorb water, so you’re slick like a seal under there. When you’re with women, you can say, “Oh ***, I am having a hot flash.’ But with all those guys, no, I am not going to say that. I just hope someone else complains about the heat so I can agree!”
Do they know?
“Do they know I’m having a hot flash?
Oh, no. I was very well trained to be the Queen of France.”
Why hide it? Every woman who lives long enough goes through menopause, and some 80% of those will have hot flashes. Why is it such a big secret?
“Everything that happens to a woman is perceived as a weakness. It’s a male culture, here in the US and in Venezuela. You can see it, she’s a b***h, but he has balls, you know? Things that happen to women, physically, are a detriment. So we hide it, no matter what.
“I sit what we call “ship-side’ with all these guys, next to the airplanes. Mechanics, VPs, execs, directors, managers, engineers, everybody is there. And 90, 95% are men. I don’t let on because I don’t want to answer their questions”not the ones they ask, and not the ones in their eyes that they don’t ask. I’m a very private person about everything, not just this. And besides, I don’t want to be responsible for educating them.
“But the problem of silence is it doesn’t do a damn thing about ignorance.
“I had other issues as well”a period that lasted an entire month, for example. When you don’t know anything, you don’t even know to ask. That can be dangerous. But my only doctor is my oncologist, so when I visit him, I only talk about the annual routine that a cancer survivor has to follow to make sure things are in check, hence, I don’t bother much to talk about menopausal issues. I don’t talk at work. I don’t talk about it either with other women outside of work. So much secrecy, taboo, stigma when we could all be sharing and be smarter. And safer.”
“I’m happy Gennev is doing this work,
I’m happy you asked me to share my story.
Together we can finally be chipping away at the ignorance.”
LL has always been a private person and doesn’t think she’d be shouting her hot flashes from the rooftops, even if it were socially acceptable to do so. But she does believe women shouldn’t have to hide the realities of their biology. A few years ago, during a meeting, someone brought up the TV show The View. The only other woman in the room, a young woman, dismissed it as “a show run by a bunch of menopausal women.” The 12 men in the room exploded in laughter.
“What did I hear? I heard, “The View? A show run by a bunch of decrepit, old women”¦’. I also heard disdain in the Millennial’s tone. I was 51-52 at the time, and not that I was menopausal, as you know my story, but I could have very well been. I didn’t say anything, but now I think I should have.” She sighs. “Like everything, you just cope,” she says. “But maybe it’s better if we work together to make it easier for the world.”
Making it easier, LL says, means helping women be comfortable with it as much as men. “I was taught to be very private in these matters, but I remember being on a camping trip with an extremely open friend. We were in our 20s (so this was 40 years ago!) and she had her period. At one point she stood up and shouted, “I am going into the woods to change my Tampax.’ I was so shocked, but the guys we were with laughed and brushed it off. So I wonder, is the embarrassment more in our heads than in the men’s?”
Ultimately, our workplaces aren’t necessarily hostile to women dealing with menopause, they’re often just casually careless. As LL says, when those in charge don’t experience it, and those who do keep it quiet, discussions don’t happen”¦and neither does change.
“I may start to challenge the silence now,” she says. “Because I have a daughter. Maybe by the time she has her first hot flash, a male co-worker will bring her ice water and that will be it.”
Are hot flashes disrupting your work and impacting your life? Speak with a Gennev menopause specialist who can help you manage your hot flashes with proven lifestyle strategies, as well as medical treatments including HRT and non-hormonal medications like Veozah.
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Oh, those glorious night sweats “¦. “I would wake up 2 or 3 times a night, roasting, my pajamas and even my sheets soaked, heart racing, panicking that I was having a heart attack. I’m a very neat person, so to wake up swimming in sweat completely grossed me out.
“I would wake up 2 or 3 times a night”¦”
“And five minutes later, I was freezing. I was changing pajamas, even my sheets, in the middle of the night, so you can guess how well my partner and I were sleeping. I finally started sleeping in the guest room because it was so embarrassing.”
Night sweats and/or hot flashes affect 75 to 80 percent of women in menopause and perimenopause, and they can go on for years. Because night flashes are so prevalent and because the disruption of sleep they cause can have so many additional negative impacts, we’ve broken down the ways you can find some relief.
What are menopause night sweats?
Oh, that flustered hypothalamus. Estrogen, the “master regulator” as neuroscientist Dr. Lisa Mosconi refers to it, is responsible for the onset of night sweats and hot flashes both.
The hypothalamus regulates our body temperature. This part of the brain has lots of estrogen receptors and hums along happily as long as the estrogen keeps coming.
But when estrogen declines in perimenopause and menopause (and less permanently, at other times of our lives), this brain structure gets confused, not sure if the body it’s regulating is freezing or overheating, and body temperature can roller coaster as the brain tries to figure it out.
The major difference between hot flashes and night sweats is really when they occur: hot flashes during the day, and night sweats at night. Night sweats (and sometimes hot flashes) can also be characterized by excessive sweating, nausea, and headaches in menopause.
How can I get night sweat relief? Some recommendations”¦
There’s no cure for the vasomotor symptoms of perimenopause and menopause, though there are ways to manage the sleep-destroying heat.
“I was changing pajamas, even my sheets, in the middle of the night”¦”
- Avoid exercise before bed. Exercise can raise the body temperature and temporarily boost metabolism, even some time later and after a shower.
- Steer clear of spicy food and alcohol in the evening. Both have been shown to trigger night sweats in many women.
- Keep your bedroom cool. A ceiling fan is great for this, as well as bedding that’s seasonally appropriate.
- Nip a night sweat in the bud. If you can interrupt the heat as it’s happening, you may be able to lessen the intensity and duration. One recent discovery we made was koldtec ice towels. They come with a flexible ice strip that you hydrate and freeze, then insert in a soft, moisture-wicking bamboo towel. Because there are six smaller ice pockets, the towel perfectly contours to the shape of your neck and stays in contact with key pulse points on your neck, maximizing the cool. The chill lasts a long time, and when the ice finally melts, the moisture stays trapped in the strip in gel form, so you stay dry. We especially love that they’re machine-washable and anti-bacterial, and that they stay frozen in their travel tube for up to 3 hours, so you can set one next to your bed.
- Wear wicking pajamas. Night sweats can pretty quickly shift to an equally miserable cold flash, especially if the pajamas you’re wearing are damp. A great brand to try is Cucumber Menopause Clothing, a line of gorgeous night wear (and, frankly, day wear as they’re that chic) perfect for women who overheat as they sleep. The great thing about the fabric is it moves moisture up and away “at speed,” so you’re not lying there in damp clothes arguing with yourself about getting up and changing. Anti-microbial, the super soft fabric holds up well.
- Invest in a cool pillow. While these pillows aren’t inexpensive, you can’t put a price on getting a good night’s sleep. These pillows are often designed with moisture-wicking materials. They draw heat away from the body, increasing airflow to prevent heat retention.
- Channel your inner cool. Meditation, mindfulness, deep breathing, biofeedback as learning ways to accept what’s happening in your body rather than fight it can help reduce the discomfort of hot flashes and night sweats.
- Talk with your doctor about medications. Antidepressants have been shown to help with vasomotor symptoms. And hormone replacement therapy (HRT) has given some women relief; just be sure to talk benefits v risks and give your doc your full medical history, especially if you have a personal or family history of clots or breast cancer.
Are night sweats dangerous?
When they’re the typical peri/menopause variety, no, night sweats aren’t dangerous. However, because they can interrupt sleep, night sweats have add-on effects that can really disrupt your life, including irritability, fatigue, brain fog, and an uptick in depression or anxiety.
However, night sweats can also be caused by thyroid issues, bacterial infections, low blood sugar, certain cancers, anxiety, and some medications. So if your night sweats come with unexplained weight loss, fever, or coughing, or come back after menopause symptoms have been gone for months or years, please consult a doctor.
Don’t sleep in the guest room. With the right combination of attitude, lifestyle adjustments, helpful products, and medications if necessary, you can get relief from the nightmare of night sweats. Speak with a Gennev doctor who can help you manage your hot flashes and night sweats with proven therapies including HRT as well as non-hormonal medications like Veozah.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Jamie, 51, checked in with us this week:
“My hot flashes in menopause feel like they’ve gone from “bake at 350″ to “broil at 500″. They’re hotter. Flaming hot”¦ Lava-hot”¦ Sweat-trickling hot. Been experiencing what I thought of as ‘hot’ for 2 years now. And lately, something inside has really cranked up the internal temperatures”¦ or, so it feels.
“I’m awake 2-3 times each night, thrashing in sweaty clothes and sheets. It’s disgusting. And then I get chilled just a few minutes later, so I’m looking for the blankets I’ve thrown off, which wakes me up even more”¦ cue the irritability.
“With all this heat, I’d hoped that at least some calories would get burned and I’d be losing some weight. Mmmmm”¦ no. Definitely not the case.” I need help beating hot flashes…
What Jamie mentioned about her temperatures rising… ahem, sparked”¦ a curiosity about heat that led us to research do hot flashes raise your temperature.
Does your temperature rise when you have a hot flash? Here’s what we found
In the National Library of Medicine, body temperatures were measured before, during, and after hot flashes in a menopausal woman. It was surprising to us that the findings shared that internal body temperatures actually fell after each hot flash.
“Where sweating occurred, the skin temperature fell during the flash and rose after it. Finger and toe temperatures always showed a sharp rise at the onset of a flash with a slower fall after the flash. Only the cheeks showed additional temperature rises; maximum, 0.7 degrees C.”
Speeding beats
Another element that was measured was the heartbeat. Is anyone going to be surprised at its acceleration during a hot flash
“The heart accelerated 13% at the onset of the flash but slowed immediately thereafter. The flash interval was sharply demarcated by undulations in the ECG baseline.”
At the core
Another study shared that core body temperature is lower in post-menopausal women than pre-menopausal women. It went on to note that this finding has potential implications for energy metabolism and midlife weight gain.
Despite all the heat and sweating we may be experiencing during menopause, our core body temperatures are decreasing as we age. Fascinating!… And it sure doesn’t feel like that mid-flash, does it?
Stress: A catalyst for hotter hot flashes?
Stress may indeed be an instigator for more and hotter flashes in some women. It’s also what we do with increased, complex, or compounded stressors that may amp up hot flash temperatures and/or the number of hot flashes that happen in a day (or night). Namely, consumables such as caffeine, alcohol, and sugar”¦ all known to affect hot flashes.
Smoking is a behavior that increases the risk for hot flashes. And, a sedentary lifestyle without much movement.
What else is going on lately in your life? Whatever the stressors, they may be impacting your menopause journey, not to mention your immune system. What are those other pre-existing stressors you’ve been experiencing, specifically? Take a deep breath, you’ve been going through a lot.
Overall health and wellness during menopause is based in good self-care
What helps? According to the same study noted above, dabbing areas of the face with cold water can provide prompt relief. It seems an easy one, as long as you’ve got cold water close at hand. Could it feel different or better than a handheld mister or handheld fan? Test drive it and see what works best, feels best, for you.
Additional areas that help decrease menopause symptoms, especially hot flashes, are:
- Nutrition in food: Aiming to get as much functional nutrition in the fuel of your food is ideal. It’s not all about perfection, or all about kale, or all about the next food trend. Take special care around sugar, caffeine, and alcohol as those can tend to increase the frequency and intensity of hot flashes. Eat more of these foods that help with hot flashes to decrease the symptoms. Overall, it’s about good fuel and feeling good. Take a look at these on-demand webinars/podcasts for ideas: this one with Dr. Ericka De Law Vella, and this one.
- Supplementation: Black Cohosh for menopause works for many women in managing hot flashes. Magnesium Glycinate is also another good one, especially to aid sleep and ease joint pain. Plus, this new daily five: Gennev’s Vitamins For Menopause Vitality pack was created for the new nutritional needs of women in menopause and midlife. Check-in with your doctor, or one of ours via telemedicine, about your current diet and what may help you.
- Water, water: Did you know that we’re more easily dehydrated during menopause than we were before? It’s true. staying hydrated during menopause is more important than ever for skin, organ and cell function, mood, and hot flash management.
- Movement: Exploring how you can move your body, all the muscles, even a little bit will help you physically, and mentally. Consider it a break, a treat, a reward, and try something new. Our Coach Stasi shares on Instagram and YouTube about this topic.
- Skip the smokes: If hot flashes are giving you grief and you’re a smoker, consider talking with others who’ve quit about their experience regarding menopause symptoms since putting down the smokes. Try it yourself, for your best health and meno-management. Estrogen and smoking puts women at risk to more likely to experience hot flashes than those who don’t.
- Decrease stress: This is a big one, and yes, it’s a general tip, but the way you decrease stress in menopause for yourself is very personal. Someone may decrease stress by meditating or yoga, another may run, another may wander through a park or on a hike, another may knit or create or write. Even incremental decreases in stress as you continue to find out what works best for you will help in managing all of your menopause symptoms.
On this note, a study shared that de-stressing may ease hot flash symptoms in some women. - Seek support: Whether it’s medical or coaching or another form of health support, more of it will help you to find practical solutions that work for your body and mind, your schedule, your family”¦ your best, whole life.
Want to try HRT for hot flashes? Or the new FDA approved non-hormonal medication Veozah? Both are effective alternatives for relieving hot flashes.. A Gennev menopause-certified gynecologist can give you a trusted opinion, determine if medication is right for you, and they can provide prescription support. Book an appointment with a doctor here.
Finding out what works for you, your body, your life is what really matters most here. Hot flashes, and other symptoms of menopause, can be managed with care and attention”¦ and of course, you’re worth the excellent care you need during this transformative journey.
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Hormonal changes caused by declining estrogen levels in mid-life are responsible for a whole festival of physical and emotional changes, including hot flashes, changes in sleep, body composition changes, dry skin, and mood swings to name a few. But here’s a bit of tasty news: By eating foods that help with hot flashes and other menopause symptoms (as well as adding a personal care system like Gennev), you might be able to avoid or reduce the severity of hot flashes.
Here’s What To Eat To Lessen Hot Flashes And Other Menopause Symptoms
Nuts and seeds to combat dry skin. Big-time almond lovers that we are, we’re thrilled almonds made this list. These foods provide healthy fats, protein, vitamin E, zinc, and fiber. The unsaturated fats in nuts and seeds can help retain the skin’s natural oils. Be sure to drink plenty of water to combat drier skin as well. Nuts and seeds are pretty densely caloric so be mindful of the portion size.
Dark leafy greens and the right fruits for better bones. Leafy greens like kale, collards, Bok choy, broccoli, spinach, and romaine lettuce are rich sources of readily absorbed calcium and Vitamin K. With the natural bone loss in menopause, it’s important to get enough calcium through the diet and/or with supplementation as needed (especially if you don’t consume regular dairy products which are high in calcium). Also magnesium, potassium and even boron are good soldiers in the fight against osteoporosis, so pile on the apples, pears, grapes, dates, and raisins.
Omega-3s to ease vaginal dryness. Flaxseed, olive oil, and some fish contain these healthy fats, so, eating more of these foods may help relieve the dryness and thinning of vaginal walls that can make everyday activities and sex painful. We also recommend adding lubricants and moisturizers like the Gennev moisture system to soothe symptoms.
Phytoestrogens to ward off hot flashes and other symptoms. Did you know soybeans have estrogen? Well, have you ever seen tofu having a hot flash? Gennev Dietitians suggest bumping up consumption of tofu, tempeh, miso, and other soy-based products as well as other phytoestrogen-containing foods like pumpkin seeds, sesame seeds, and sunflower seeds, celery, rhubarb, and green beans. Because these foods contain estrogenic compounds, they can relieve some of the symptoms caused by estrogen decline.
Proteinasnatural aging and estrogen decline causes a decrease in lean body mass (muscle loss) and protein is needed to maintain or grow that mass (together with exercise-specifically strength training). Gennev Dietitians suggest including either lean animal or plant-based protein to most meals and snacks to support maintaining muscle and helping with satiety, or feeling full.
Cool off those hot flashes starting now! Our Registered Dietitian Nutritionists are trained to support you in menopause. They will create a personalized nutrition and wellness plan to help relieve your symptoms, so you can thrive starting now.
Avoid These Foods to Help With Hot Flashes & Other Menopause Symptoms
During menopause, some foods are probably best avoided, or at least minimized, as they can make symptoms worse.
Coffee, caffeine, alcohol, chocolate, the spicy stuff. We know”add in a movie with Ryan Reynolds in it, and that sounds like a terrific Friday night. But while hot flashes are a problem, spicy foods, can all trigger a rise in body temperature. And you may not be sleeping all that well right now, so reducing caffeine could help that too. Ryan Reynolds movies, however, are not only OK but downright encouraged. Every woman’s body is unique and will have different food triggers so this may take some experimenting.
Sugar. If you find you’re tired a lot, the rises and dips in energy may be partly due to too much sugar in your diet. Fruit naturally contains sugar, but the water and fiber that go with it can help regulate your body’s absorption of sugar, so when you’re jonesing for something sweet, opt for a handful of frozen grapes or a really good peach instead. Since many women find it harder to maintain their weight when estrogen levels decline, ditching the donuts can have add-on (or don’t add on, in this case) benefits.
White carbs. The more processed the food, the easier it is for your body to process the calories from it. That’s why Dietitians recommend whole grain versions of your favorite carbohydrates. You’ll feel fuller longer and get more nutrition from whole grains like brown rice and whole-grain bread or whole wheat pasta.
Hot flashes just won’t quit? Speak with a Gennev menopause specialist who can help you manage your hot flashes with proven lifestyle strategies, as well as medical treatments including HRT and non-hormonal medications like Veozah.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“