While menopause is a normal and natural part of aging for women, many of us have no idea what to expect as we approach our post-reproductive years. And many symptoms that can accompany menopause, along with their impact on our bodies, minds and emotions, can leave even the strongest woman feeling alone. Because the topic of menopause was, and is, still widely considered “taboo” or “off limits” for our mothers, and our mother’s mother (and so on), many of us find ourselves part of a tribe of women lacking the passed-down knowledge that could make all the difference for how we approach this inevitable time of our lives.
One of the most powerful aspects of the Gennev brand is the community of women who gather with us, finding common ground with other women through shared experiences, offering advice and gaining support from someone who “gets it”. We have made it our mission to educate women about menopause. Our wish is that women will be part of the change, and help us pass on menopause knowledge to future generations.
We asked the Gennev community what advice they would share with younger women about what to expect in menopause. Below are their responses.
It’s so much more than hot flashes
“First of all, it is important to talk about strange symptoms you are experiencing. Ask questions, do not be ashamed and see a trusted GP that will help you through it. Be brave and know that you are not alone”¦” Mauricia B, 48 Perimenopause
“Menopause is NOT just about hot flashes. There are a lot of symptoms to consider that can impact your long-term health during perimenopause and menopause. I started experiencing perimenopause at age 43 and left it to fester until it was unbearable at age 49. I wish I had taken it seriously while I was knee-deep in perimenopause.” Valerie W, 58, Postmenopause
“Menopause is so much more than just not having a period. It involves the mind and the body and the changes are different for everybody. It’s important to take very good care of oneself, eat properly, continue to move and exercise and to keep the brain active. I would recommend trying the least invasive things first to relieve uncomfortable menopausal symptoms. If that doesn’t work then try hormone replacement therapy and keep checking in with yourself. It helps to discuss menopause with other women that are going through or who have been through similar circumstances.” Terry C, 56, Postmenopause
“It’s a natural progression in the life of a woman. Learn as much as you can in your thirties so that you’re prepared and aren’t overwhelmed by the changes that will take place physically, mentally, and emotionally. Talk to other women about their experiences if they’re open to it.” Anonymous, 63, Postmenopause
“It creeps in on you and starts earlier than you might expect”¦!” Anonymous, 49, Perimenopause
Don’t suffer through symptoms, and seek menopause care
“If you have an OBGYN, expect to explore a gynecologist with specialty in menopause. Doctors are never taught menopause. And they themselves don’t know very much about it for themselves. Don’t expect the doctors to have the answers. They don’t. Mine told me I was crazy – what I’m experiencing is due to stress, travel, work, etc. Not perimenopause even though I knew in my gut that this wasn’t just life circumstances and choices. It was a shift in my body make up. Trust your intuition.” Anonymous, 46, Perimenopause
“Hormones havoc the lives of women to such an extent that we find no road, but stay calm, till the symptoms subside on their own – it might take years of our life, nothing is in our hands except the lifestyle changes and positive approach towards the transformation we have.” Anonymous, 50, Postmenopause
“Don’t suffer with symptoms; blood tests do not give the full picture; arm yourself with information.” Anonymous, 45, Perimenopause
“It has helped me to just dive into learning about it. I’m also reminded of the quote that goes something like “the only thing certain in life is change”. I’m working on embracing and finding the positives in the changes. For me, getting to this stage of life means I have a lot more freedom and options of how I spend my work time and free time. That’s definitely a positive aspect of all of this!” Anonymous, 42, Perimenopause
“Expect that you will probably be in perimenopause long before you think you are, and that even if you have a female doctor, they might not be able to give you the correct or all the information you need. They may not know any better of what is happening to you. So, READ whatever you can about perimenopause, menopause, etc. Don’t be afraid to talk with your friends. I’ve found that when I bring up what I’m going through, so many of them are willing to open up and seem almost relieved to have someone else to talk to. You’re not alone!” Lisa H, 50, Postmenopause
“Expect! I’d tell all start now! Ask your mother and also if you have a grandmother, your aunts. Plain as can be I say look for reputable menopause research.” Ginny K, 63, Postmenopause
“Totally natural process but there are so many different ways each woman goes through it. For me having a close friend also going through it helps. We talk to each other about it also.” Annalise S, 46, Perimenopause
“Expect your body’s “normal” patterns to change – some changes will be annoying and frustrating and some will be a relief. Don’t freak out but do check in with your doctor because there might be something else exacerbating your symptoms. Embrace the transition from being the fresh-faced newbie into being the mentor who can give wise guidance. You have a lot to offer the world even if no one else is validating that right now. Your creative energy may shift in a new direction and that is okay. It’s okay to stop chasing youth and embrace your scars, and grey hair, and laugh lines – let your character show.” Angela S, 47, Perimenopause
“Everyone’s body is different and will experience different symptoms. When you feel like you’re at your ropes-end, press forward with all you got.” Anonymous, 43, Perimenopause
“Read, learn, discuss with those who you know who have experienced it because it WILL happen to you.” Jennifer F, 53, Perimenopause
“It is different for everyone. You are unique and need to know yourself and your body. Reach out for help. Hormones are real. They do run our lives ….. :-)” Lisa J.B., 53, Perimenopause
“Hot flashes are no joke, so dress in layers. And, don’t be ashamed or afraid to talk about it. Menopause was always something I thought of happening when I’m “old” but at 52 I’m not old at all. I’m healthy, vibrant, fun & fun-loving. I’m strong and sexy and smart. It can certainly be a bit of a roller coaster, but talking about it, sharing your experience and finding some humor in it can all be healthy and therapeutic in managing it. And the more we, as women, talk about it the more it’ll become “normal” vs taboo or something that signals “old age”. It’s just a stage that we all go through. And the best part? Never having to worry about your period again. You can wear whatever you want, white pants and all, whenever you want! Not gonna lie though, I’ll be glad when the hot flashes are over…” Erin E, 52, Postmenopause
“Expect your journey to be your own. Expect to get help so demand it. Expect to be amazed and empowered by the women you’re in it with!” Jenn K, 50, Perimenopause
“I would advise to expect a period like your teenage years with a lot of hormones imbalance so I would advise them to get ready early as possible with lots of information to be able to prepare your body and your mind, and don’t think of menopause as a taboo because it doesn’t represent the end of our life or something to be ashamed of. And I really hope that soon GPs could be more knowledgeable about it and be more supportive because we really need it.” Orietta F, 52
“Read all you can about it. It’s been really rough for me, but knowledge has helped me know how to help myself.” Paula C, 50, Perimenopause
“Be aware that any physiological and/or psychological changes from your mid 30s could be hormone-related. The symptoms of perimenopause are so wide-ranging and vary from woman to woman but, certainly, if you were previously a happy, optimistic person and suddenly realize you are feeling low and/or anxious for no particular reason, this could be a sign that things are starting to change.” Louise S, 44, Perimenopause
“Take extra good care of all parts of yourself. Emotionally, physically and spiritually. Address underlying issues, don’t let things be swept under the rug.” Tanya C, 53, Perimenopause
“Don’t dread it, but instead inform and arm yourself with information and stories from other women. Women don’t need to suffer; there are so many ways to feel really amazing in your body. This time of life is too precious not to live to your fullest.” Jill A, 47, Perimenopause
“I was afraid to talk about it. My kids were in their late teens and early twenties, every time the “M” word came up they would tease and joke about it excessively. I would not talk about it, but I finally got fed up and told them it was hurtful and isolating. That changed the entire concept of menopause for all of us. I did not want to be “old” enough to be perimenopausal! Acceptance made the process so much easier.” Dana H, 52, Postmenopause
“Find someone supportive to talk/cry/laugh with. My sister and I lean on each other.” Lisa C, 57, Postmenopause
“Be good to yourself, even though it’s hard, embrace the changes in your body and try to deal with relations issues as best you can before you are officially in menopause. I found the things I didn’t deal with before in my life came at me bigger and worse than ever. Really had to cut some ties this year, grieve a lot and make time for myself to stay as calm as possible.” Laurie C, 59, Postmenopause
“It can start as early as your 30’s. Talk with your mother/aunt/grandmother about the issues they experienced. Educate yourself and empower every young woman to do the same.” Deborah B, 57, Postmenopause
“When you start to experience symptoms that aren’t “you” – brain fog, irritability, low energy, mild depression, increased anxiety, wonky periods – don’t let your provider tell you: “You’re too young to be experiencing perimenopause.” Go online and search for a provider that specializes in menopause symptoms and treatment, because you’re going to need her expertise for the next decade or more. Starting early will mean you’re not caught unaware and alone in the journey every woman takes. You will have education and support.” Dessie, 51 Perimenopause
Be part of the change in educating women about menopause
Join us in being part of the change! Share these 28 responses along with your own menopause experiences with the younger women in your personal community. We all menopause better together!
There are over 34 symptoms that women experience throughout menopause. From hot flashes, weight changes and sleep disturbances, to vaginal dryness, mood swings and fatigue, hormonal shifts are something you can expect in menopause! There’s no need to grin and bear the symptoms of menopause. Gennev’s board-certified OB/GYNs specialize in menopause and will help you understand your symptoms and find relief with prescription or natural therapies that are right for you.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Many women in midlife suffer from trouble falling asleep, staying asleep, and low energy during daytime hours. As we age our sleep patterns change. A key contributing factor to quality sleep is our level of melatonin. Melatonin is a hormone made in the pineal gland that helps to regulate our sleep-wake cycles. Melatonin is well-known to promote sleep, maintain sleep, reset the circadian clock and improve sleep quality in general. And as you may have guessed, our melatonin production declines as we get older.
A great place to start in improving sleep quality is practicing good sleep hygiene:
- Get outside daily for some movement in the daylight hours
- Try to keep a healthy sleep cycle that allows plenty of daylight exposure to your body (sit by a window at work, take a walk).
- When you settle in towards bed, avoid screens. Dim the lights, close the curtains, make sure there are no lights in your room.
Before turning to a sleep aid, you should consider all the things you may or may not be doing that influence your sleep. Sleep troubles can be attributed to your diet, exercise habits, stress management, alcohol and caffeine intake, medications, underlying medical conditions, hormone fluctuations (hello hot flashes!) room temperature, room darkness, and more.
And when good sleep hygiene is simply not enough, there’s now Gennev Sleep.
Introducing Sleep
We asked Naturopathic Physician, Dr. Wendy Ellis, to formulate a sleep supplement that would support women in menopause. She chose these ingredients for our sleep formula based on her 20 years of clinical experience with various sleep products and single ingredients. She shared, “I love this combination as it helps with falling asleep, but also staying asleep, with the added benefit of reducing anxiety and inflammation.”
Sleep’s proprietary formula provides the following benefits:
- A safe, effective way to help slow down racing thoughts at the end of the day
- Experience a relaxed mood that eases you into a better quality of sleep
- Non-addicting, non-drowsy, and provides immediate relief
What is in Sleep
Sleep is a proprietary blend of Melatonin, 5HTP, L-theanine, and Magnolia.
“Melatonin as Sleep includes only 1mg of melatonin to help you fall asleep. Peak concentration is within one hour of taking melatonin, but the effects begin as soon as 20 minutes after taking it, and it stays in your system for 4-5 hours. We kept the dosage of melatonin in Sleep to this low dose, as too much melatonin can contribute to nightmares, waking after 3-4 hours, and may leave you feeling groggy in the morning.
5HTP as is an amino acid. It is the precursor for serotonin and melatonin, thus it influences mood and sleep in a positive way. By providing 5HTP to the body before bed, you’re providing more of a foundation for your body to produce serotonin and melatonin.
L-theanine – is a unique amino acid that is naturally found in tea plants. It is one of Dr. Ellis’ favorite amino acids for treatment of menopausal sleep issues because it also has anti-anxiety properties. Amino acids such as 5HTP and L-theanine are a very safe, effective way to treat mood and sleep disturbances. It’s sedating without creating daytime drowsiness, helps slow down the ruminating women often feel at the end of a long day, as well as improving the quality of sleep.
Magnolia – This very safe botanical was added due to the effects it has on our “calming” neurotransmitter, GABA. It helps to create a relaxed mood that allows women to fall asleep more quickly, as well as improve the quality of sleep, without negative side effects.
The best way to take Sleep
Take only 1 capsule of sleep per day, approximately 15 min before you want to fall asleep.
Talk with your physician before taking Sleep to avoid interactions with other medications, and especially antidepressants (SSRI/SNRI).
Most sleep issues are behavioral, meaning it’s better to figure out the root cause of insomnia, instead of taking a sleep aid every night. That being said, sometimes you may need to take it for a few nights, weeks or even months in stressful periods, and this is absolutely fine!
Safety:
- Vomiting and nausea have been reported when 5-HTP was taken in excess of 100 mg in some people.
- 5-HTP can cause serious drug interactions with many medications, especially those used to treat depression. Because antidepressants generally work by increasing serotonin in the brain, 5-HTP could combine with these medications to cause high concentrations of serotonin.
- Having too much serotonin can lead to serotonin syndrome, a serious condition characterized by dangerously high heart rate, blood pressure, and temperature. 5-HTP can interact with other classes of drugs, like migraine and pain medications, that also affect serotonin concentrations.
- Taking magnolia bark along with drugs that promote sleep or treat anxiety, such as sedatives, sleep medications, and barbiturates, may cause drowsiness. Taking magnolia bark with blood thinners, including aspirin, is not recommended. It may increase the risk of bleeding. See this reference for more information.
Dr. Ellis shares, “The formula for Sleep not only helps you fall asleep, but stay asleep, with the added benefit of not feeling “hung over” in the morning. Sleep is a non-addictive formula and has a great safety profile.”
If you continue to have sleep issues, consider seeing a board-certified sleep specialist or a behavioral sleep specialist. They can provide cognitive behavioral therapy, which has been shown to be effective for chronic sleep problems. Always check with your doctor before taking any new supplements or medicines.
When you notice a change in sleep pattern that may be associated with the menopause transition, especially if body temperature instability is part of the problem, consider an appointment with a Gennev doctor to address the role that hormonal shifts can play in your trouble sleeping.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
When we asked women this past year what they knew about menopause before starting their own journey, their answers were overwhelmingly, “not much”. Beyond hot flashes and night sweats as well as no more periods, many women were unaware of what to expect, and were caught by surprise by the widespread impact on their bodies and emotions. One woman commented that she thought menopause was something that “just sort of happened”. “¯She shared, “I guess like when I got my period for the first time – it started without warning. So [I thought my periods] would just stop, and there would be much rejoicing.”
We followed up with the question of what surprised them most about menopause. And their answers were just as unique as the experience of menopause is to every woman. While the majority of respondents answered that they suffered with multiple vexing symptoms, we were delighted to hear it wasn’t all bad. Some women are also finding the silver lining in this transitional stage of life. As one woman put it, “Menopause isn’t just one thing, but many experiences. And it doesn’t have to mean that I’m old or past my prime. I can still feel good and vibrant and have energy. Weight gain isn’t inevitable and CAN be controlled. I can build endurance and strength if I carve out the time. And I’m worth the effort. That said, the inability to sleep soundly and consistently has been the hardest and most frustrating aspect of menopause.”
Women learn from other women’s experiences. And feeling like you are not alone in menopause can be very good for your emotional health. Here are 25 surprising things women shared they have experienced with menopause.
What has been the most surprising aspect of menopause?
- “How much the change in hormone levels affects every aspect of your life.”
- “How my body and brain are fairly unrecognizable when compared to my body and brain of even 12 months ago.”
- “Hair loss, sleeplessness, forgetfulness, belly fat (even though I never had children).”
- “Mood changes, joint pain, itchy & dry skin, scalp hair changes, breast cysts forming, vaginal dryness, digestion slowing down, that it can start many years before actually stopping!”
- “The most surprising aspect has been how hard menopause hit my body. I’ve always been blessed with good health and an active lifestyle. I never expected to develop vertigo, an anxiety disorder, or have my nervous system feel like it’s on fire. I never thought it would disrupt my life as it has. And I never thought I would fight with my body so much.”
- “I was most surprised that my OB/GYN really couldn’t help with this aspect of my health. Not a lot of knowledge about menopause and she did not have the time to review all the options out there for me to explore like HRT, supplements, and lifestyle changes.”
- “That I started perimenopause WAY, WAY before I even knew what was going on with my body. I had no idea why I felt the way I did, and why my periods were so terrible for so many years in my early 40’s. How tired I would feel. How it would affect so much of who I am; my confidence, my sex drive, my energy level, and don’t get me started with the brain fog. So much brain fog. It’s scary.”
- “That it happened so early.. also Lichens sclerosis.”
- “I’m amazed that my sleep is now so compromised. I can fall asleep no problem, but staying asleep is a challenge.”
- “How it has affected my life as far as having brain fog, anxiety, ringing in my ears.”
- “That at a certain point you start experiencing a lot of different symptoms, some days more some days less, your body starts changing and your brain too…and you start asking yourself what’s going on? After a while you ask yourself why nobody told me about this?”
- “The feeling that my body has lost control of its normal disposition. I experienced extreme anxiety attacks, palpitations and an elevated heart-rate. Nothing I had heard of being the typical menopause symptoms”¦”
- “I get nauseous right before a hot flash.”¯ Also, how night sweats come one right after the other and I haven’t slept in weeks.”
- “Crawly skin, tingling and pins and needle.. heavy head/burning scalp/ and muscle weakness to name a few.”
- “To lose my eyebrows”¦ and grow facial hair on my lip and at the side of my face.”
- “Neurological symptoms: brain fog, mood swings, depression.”
- “It totally sucks! I hate not feeling in control of my moods or my body!”
- “My biggest problems were the symptoms I did not attribute to menopause.”¯ I was deeply concerned I was in early onset Alzheimer’s.”¯Unable to find words, not complex words but everyday nouns.”¯Both of my Grandmas had Alzheimer’s, but not at the age of 50.”¯ The utter relief I felt after learning this happens in menopause, I can’t even describe how I felt!”
- “Anxiety. Major mood swings. Emotional rollercoaster. No libido.”
- “How fast it has hit me. And the amount of discomfort I have in my feet and legs on a daily basis”
- “Loss of words, hairs in new and unwelcome places, the sudden onslaught of anxiety over unfixable past actions, social anxiety, and the sharp increase in caring what others think of me.”
- “How absolutely out of control I feel. I have been suffering from such random symptoms like rashes, headaches,”¯ heavy periods, joint pain, anxiety,”¯ depression, weight gain. I thought I was going mad! I am 48 and I feel like an old woman. A few months later, I realized that I was in real trouble when I started feeling anxious and depressed. Please note that I have never ever suffered with either.”
- “I LOVE being the AGE of menopause.”¯ I wish I had more answers so I could move through it with more clarity.”¯ I’d love to feel like I had more control.”
- “The increase in confidence in who I am and what I have to offer, and I pick things and activities because I like them, not because of how others will perceive me.”
- “The freedom and empowerment.”
Your menopause journey is as unique as you are. And while some symptoms are more common than others, our integrated menopause care team is trained to support you through them all. Join the 94% of women who have found relief in menopause by visiting with a Gennev board-certified OB/GYN who specializes in menopause.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Having a healthy gut is integral to overall wellness. Gut health is linked to not only your digestive system, but also plays a role in metabolism, glucose tolerance, insulin sensitivity, the nervous system, endocrine system, and more. The gut microbiome is made up of trillions of bacterial cells, fungi and other microbes, and is as unique to you as your fingerprint. Your unique microbiome began development in utero, and is influenced by many factors including but not limited to genetics, a vaginal or cesarean birth, breastfeeding, the environment, exercise and sleep habits, hormones and nutrition. The bacteria in the gut serves as a communicator to other systems in the body. Changes in the bacteria in the gut microbiome can disrupt the messaging function and put you at an increased risk of many systemic conditions including cardiovascular disease, irritable bowel syndrome, type 2 diabetes, mental health concerns, and auto-immune disease.
Menopause and the microbiome
There is evidence that suggests hormone fluctuations and specifically the decrease in estrogen, influences the microbiome by altering the bacteria that is present in the gut. We also know that estrogen receptors are located in the intestines, brain, bones and adipose tissue (commonly known as body fat). While it is too soon in the research to know if there is a direct relationship between hormone mediated changes in the gut and menopausal symptoms, it is hypothesized that the microbiome may play a mediating factor in body fat increases, cardiovascular disease, and cognitive decline.
Many women suffer from digestive issues in menopause. This may be attributed to the decrease in estrogen slowing down the motility of the digestive tract, which commonly leads to bloating, gas, and constipation. The hormonal shifts contributing to a change in the bacterial make-up of the gut may also result in poor digestion. The increased stress experienced by many women during menopause can also impact the gut microbiome. The bacteria in the gut communicates with the brain bi-directionally through the gut-brain axis. So if you are experiencing intestinal or digestive distress, it can be the cause — or the result –of anxiety, stress, or depression.
It’s probably not surprising that the lack of sleep common with menopause can also impact the gut microbiome. Add in the increased stress from multiple nights of poor sleep combined with all of the above and you have a perfect storm for a less resilient, less diverse microbiome. There are, however, ways to support your gut health and mitigate these effects.
Essentials for a healthy gut microbiome
A diverse gut is a resilient gut. With an increase in bacterial diversity in the gut, the body becomes more resistant to illness, cardio-respiratory fitness and metabolic health are optimized, and exercise performance is elevated. So how do you create a diverse, healthy gut?
- Eat a diverse diet. Gennev supports a food-first approach. A variety of whole foods is key for gut health, mainly from plant sources like fruits, veggies, legumes, beans, and whole grains. “
- Fill up on fiber. The resistant carbohydrates found in vegetables, fruits, and whole grains provide bacteria to contribute to the diversity of the gut. “
- Fermented foods like plain yogurt, kefir, Kimchi, and sauerkraut benefit the gut by contributing optimal beneficial bacteria in the intestines. “
- Prebiotics help feed the bacteria in your gut and may promote the growth of specific beneficial strains. Some popular prebiotic foods include whole grain oats, bananas, apples, garlic, onion and asparagus. “
- Eat the colors of the rainbow. Colorful fruits and vegetables offer phytochemicals (plant chemicals) which can contribute bacteria that helps manage inflammation and mitigate bacteria associated with poor health. Blueberries, raspberries, herbs, and lettuce are great sources of phytochemicals.“
- Get your omega-3s. Similar to colorful foods, foods containing omega-3s also support the production of anti-inflammatory compounds in the gut. Salmon, anchovies, sardines, walnuts, chia seeds, flaxseeds, and hemp seeds are all great omega-3 sources. “
- Exercise. Studies have shown that regular exercise helps to aid in digestion and promote the resiliency of the gut. “
- Meditate and prioritize sleep. Both of these activate the parasympathetic or ‘rest and digest’ response through the gut-brain axis mentioned above. Calming the mind and the body supports a more optimal gut environment.
When it comes to gut-healthy foods, keep it real, and a little dirty. Eat more plants that are organic or locally grown if you can. And when you are washing your veggies and fruit, a light rinse with water and a rub will suffice. No need to use soap or vigorously scrub as you may lose some of the beneficial bacteria.
Most importantly, have fun in the kitchen! As you transition your meals to include more plants, see how many you can tally in a day. Small additions can add up quickly as you diversify your diet. Smoothies are a great way to load on beneficial ingredients. And try acai bowls, or grain or salad bowls, where you can layer on beneficial ingredients and gain gut health rewards.
You want less of these for a healthy gut
- Processed foods
- Refined sugar
- Saturated fat
- Artificial sweeteners
- Stress
In high amounts, these tend to decrease the diversity of the gut microbiome. While it is near impossible to eliminate these all together, it is recommended to limit your intake and prioritize what to add more of. If possible, limit the use of pain medications, NSAIDs and PPIs as they similarly can decrease diversity of the microbiome. Speak with your physician before changing anything to your prescribed routine as the benefits of these medications may outweigh the impact on your microbiome.
When your gut microbiome feels off, you may be tempted to try the next new thing that comes your way. From probiotics and other supplements, to microbiome testing, there are plenty of new products hitting the market to tempt you. We suggest using a food-first approach as your foundation for a healthy gut. A diverse diet with a variety of foods is key “ even with probiotics. And most importantly, with microbiome testing – always check-in with your body. This area of study is still quite new, so approach with curiosity and keep an open mind. And be critical about the results to be sure they fit with what your gut is telling you.
If you need support in managing your digestive health, Gennev’s integrated care team can help you create a personalized plan designed to meet your wellness goals. Our dietitians have specific microbiome training to help you diversify and optimize your gut health.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
Weighing the benefits and risks of hormone replacement therapy (HRT) related to menopause can be one of the most confusing decisions a woman will make over the age of 50. There is no one-size-fits-all recommendation that can make the choice simple, or standardized chart to reference “if this, then that” scenarios. Every decision about HRT should be individual, and best when made between a patient and her health care provider.
Additionally, the care and treatment of menopausal women is complicated by the varied level of training and specialized experience of health care providers related to menopause. Not all OB/GYN’s or other health care providers have studied the latest research related to the potential benefits and risks of HRT in accordance with personal and family health history – research that increasingly demonstrates a window of time where HRT can provide both symptom relief and, in some cases, delay or ward off disease.
Most problematic is the legacy effect of how providers understand and interpret the seminal research that has been the basis for standardized care for HRT”a study completed two decades ago”called the Women’s Health Initiative (WHI). The 2002 study was conducted with women at an average age of 64- 65, and cited health risks associated with HRT around cancer, blood clots, and heart disease. Many healthcare providers have not kept up with subsequent publications on this data that showed that in women who were younger when they started, the risks are fewer and benefits greater. This has come at a cost to menopausal women suffering from sleepless nights, brain fog, painful sex, and hot flashes.
Thankfully, attitudes are shifting as new research surfaces. Both the Endocrine Society and the North American Menopause Society state that for symptom relief, the benefits of FDA-approved hormone therapy outweigh the risks in women younger than 60 or within 10 years of their last period, absent health issues such as a high risk of breast cancer or heart disease. The menopause society position statement adds that there are also benefits of HRT for women at high risk of bone loss or fracture.
With a bit of education, and having an informed conversation with a doctor, OB/GYN, or a menopause specialist, women are moving beyond the decades-old stigma of the HRT health concerns. They are creating personalized preparedness plans with their doctors as to when hormone therapy, if used as directed, might deliver more benefits than risks.
3 questions to ask your doctor about HRT
To evaluate with your doctor whether hormone therapy could be right for you, at what age, for how long, and what type, see the below set of questions and considerations to review in advance of your appointment, or to guide conversations with your doctor.
Based on the severity of how my menopause symptoms are impacting my quality of life and daily routine, would HRT potentially deliver relief?
- There are 40+ symptoms associated with menopause. The most common include hot flashes, vaginal dryness, painful sex, insomnia, fatigue, headaches, joint pain, anxiety, mood swings, memory lapses, digestive problems, and brittle nails.
- It is up to each individual woman to decide when and how her symptoms are impacting her quality of life and need addressing to provide relief.
- As some of the above symptoms can be related to other health issues, it is helpful to discuss which tests and screenings could be done to rule out other health concerns.
How might my health history, and that of my family, such as heart disease, strokes, dementia, osteoporosis, etc. factor into the benefits or risks of HRT?
- HRT may be especially beneficial if you have a family history of”¯osteoporosis, high”¯cholesterol, and”¯heart disease. On the other hand, it may not be best if you have”¯gynecologic cancer,”¯ or a blood clotting disorder.
- There is increasing evidence that starting HRT at the transition to Menopause can reduce the risk of Alzheimer’s, as discovered in studies by Dr. Lisa Mosconi.
- Research on cardiovascular health shows increasing evidence that starting HRT in the early years of menopause can provide cardiovascular benefit with reduced risk of cardiovascular disease. This benefit changes with age, and HRT may become riskier as you get further into menopause.
- There is evidence that HRT can help prevent osteoporosis.
- If you still have a uterus, Progesterone is recommended along with Estrogen to avoid the risk of uterine cancer. However, progesterone does slightly impact the incidence of breast cancer. The increase in risk is actually very low.
- If you have a family history of breast cancer, hormone therapy will not impact your risk (which is based on family history and genetics), and may be a valid choice for you.
Given my symptoms and family history, why type of HRT is best and for how long?
- Some of the options for HRT include topical, vaginal, oral pills, and patches”all with pros and cons and are described here.
- FDA regulated forms are always safest, and your doctor should be recommending these.
- Length of use of HRT is based on your symptoms and benefits from HRT, and varies woman to woman. There is no set stop date or number of years after which you must stop.
As research continues to emerge that demonstrates the benefits of hormone therapy for short term symptom relief and long-term risks related to heart, bone, and brain disease, there is no doubt decision making will become easier and standards will shift. Until that time, women at the age of 45 can have a conversation with a Gennev OB/GYN or their physician about how HRT might be considered as they move through menopause, and under what scenarios. This can set a valuable benchmark to inform treatment, if needed, in line with their own personal and family health history, and their individual health goals.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Joanna Wasmuth has always juggled a variety of roles and responsibilities, producing impressive results in her career while lovingly taking care of family and friends. Like so many women, Joanna has spent so much time and attention on others that she neglected herself – until now. Joanna has taken her strong work ethic, care, compassion, and business savvy and applied it to a new, and probably the most important job of her life”CEO of her health. “I need to be responsible for my own health,” Joanna says. “Your doctor doesn’t live in your shoes. While they’re wise and have great input, we also have to trust our intuition.” And with all the varying symptoms that accompany menopause, advocating for yourself and seeking the care you deserve is more important than ever.
Today, Joanna’s prioritizing herself, her health, and finding peace and joy. But just a few years ago, she was driven to produce, often putting herself last. Joanna was on a plane several times a week, flying around the world for her job as a strategy consultant, commuting between her home in Miami and office in New York City. She was also making cross-country trips to Seattle to care for her mom and sister, who were both ill. There were early mornings, late nights, and lots of stress. “I was running myself into the ground,” she says.
Everything changed when, at age 44, Joanna had a hysterectomy that included the removal of her ovaries. “I was told that I’d just be put on an estrogen patch, and life would be normal, no big deal,” she recalls. Four day slater, Joanna had three life-threatening pulmonary emboli (blood clots in the lungs) and landed in the ICU. She not only faced months of recovery from that emergency, but she was plunged into surgical menopause with intense symptoms like debilitating joint pain, hot flashes that felt like she was “claustrophobic, suffocating, and burning from the inside out,” sleep problems, weight gain, and memory issues. And because of the pulmonary emboli, hormone replacement therapy was no longer an option.
“I realized that now my body is different, and I couldn’t just keep doing the things I used to do,” says the now-46-year-old. Thanks in part to the pandemic, she’s doing more Zoom meetings and traveling less, which has reduced her stress. “I’ve been given a second chance at life, and having beautiful moments every day is what I’m looking for now.”
As the CEO of her health, Joanna has employed some of her business systems and management skills, starting with a spreadsheet of non-negotiables. “What gets measured gets done,” she explained as she shared her list of 28 “things that I do to be well.” Some are daily practices like drinking 100 ounces of water, walking four miles (she uses the Conqueror virtual challenges to stay motivated and keep it fun), cooking plant-based meals, painting, and meditation using sound bowls (“It’s just a few minutes of peace and resets my energy”). Others are weekly rituals, for instance, meeting with her Gennev health coach to stay on track, sessions in an infrared sauna, sound and light therapy, and strength training (three times a week). And monthly, she gets a massage, has acupuncture, and meets with a Gennev menopause-certified doctor. She marks off each goal in the spreadsheet as she goes, to help her stay on track.
She’s also adjusted her day to have breaks between meetings instead of scheduling them back-to-back. And when she has a stressful presentation or appointment, she rejuvenates by doing something that brings her joy, like walking on the beach or spending time in a favorite place. “As we do hard things, we can do them in a way that supports our wellness and our health,” Joanna says.
Joanna’s return on her investment has surpassed expectations, as her doctors frequently express amazement with how well she’s recovering. She’s a perfect example that no matter how bad the symptoms are, you can find a way to thrive. “This is a season of life where it’s not the end, it’s a new chapter,” Joanna says. “And it can be an exciting one.”
If you connected with Joanna’s story, and need support in taking charge of your own health in menopause, book a virtual visit with a Gennev menopause specialist.
“
The information on the Gennev site is never meant to replace the care of aqualified medical professional. Hormonalshifts throughout menopause can prompt a lot of changes in your body, andsimply assuming something is “just menopause” can leave you vulnerable to otherpossible causes. Always consult with your physician or schedule an appointmentwith one of Gennev’stelemedicine doctors before beginning any new treatment or therapy.
“
The Mediterranean diet is more of an eating style than a diet. It incorporates a variety of whole, nutrient-rich foods that provide the nourishment important for promoting heart health, reducing inflammation, stabilizing blood sugar, managing weight, and more. There are no strict rules for the Mediterranean diet, as it is based on the traditional foods and eating style that people eat in countries bordering the Mediterranean Sea (including France, Spain, Greece, and Italy). Since many people find themselves unsure of how to get started with the Mediterranean diet, we’ve broken down the basics below. One key to keep in mind is that the less processed and more whole a food is, the more likely it is to fit into the Mediterranean style of eating.
The basics of the Mediterranean diet
Create a colorful plate. Brightly colored vegetables and fruits provide many of the benefits found in the Mediterranean diet. We also eat with our eyes, so see what you can do to have at least five bright colors as the main part of your meal.
Choose fish more often as your animal protein source. Chicken, turkey, eggs, cheese and yogurt are also excellent sources of lean protein, but most of us don’t consume an optimal amount of omega-3s from our food which is what fish can provide. .
Include plant-based proteins. Lentils and beans are fabulous sources of protein and fiber. Enjoy hummus made from chickpeas or a lentil soup a few times per week.
Prioritize healthy fats. Unsaturated fats from fresh salmon, nuts, and seeds provide nutrients that can support the body’s ability to manage inflammation. In addition, these foods are also a good protein source. Olive oil is a main staple in the Mediterranean diet. Use this to prepare salad dressings, marinades, and to cook with.
Go for whole grain. Whole grains such as quinoa and brown rice provide more nutrients, fiber, and protein compared to simple and refined grains. These can also be prepared easily in a large batch and added to meals throughout the week such as a salad for lunch to bring to work or a way to round out a dinner.
Don’t skimp on flavor. Use fresh herbs, garlic, lemon juice, salt, and pepper for flavor. These simple, fresh, and nutrient-rich ingredients can really pack a pop of flavor and offer anti-inflammatory benefits that often go unrecognized.
Eat more of these foods when following the Mediterranean diet
Vegetables and Fruits as Aim for half of your plate to be filled with fruits and vegetables
- Arugula
- Kale
- Spinach
- Romaine lettuce
- Red peppers
- Carrots
- Cabbage
- Radicchio
- Blueberries
- Apples
- Bananas
- Oranges
- Pears
- Strawberries
- Grapes
- Dates
- Figs
- Melons
- Peaches”¯
Whole Grainsas ¼ of your plate should consists of whole grains
- Oats
- Brown rice
- Quinoa
- Farro
- Bulgur
- Whole wheat pasta, bread, crackers
- Rye
- Barley
Lean Proteins (animal or plant) as ¼ of your plate should consist of healthy protein
Animal Protein as strive to eat fish or seafood at least twice per week, and include a protein source with all meals and snacks
- Wild caught salmon, tuna, trout, mackerel, herring
- Canned tuna, salmon, sardines, anchovies
- Chicken
- Eggs
- Turkey
Plant protein
- Nuts/nut butter (almonds, walnuts, pistachios, peanuts, pecans)
- Beans (black, kidney, garbanzo)
- Peas
- Lentils
- Tempeh
- Tofu
Healthy fats as add the following as a condiment to meals as or as part of the preparation
- Olives and extra virgin olive oil
- Avocados and avocado oil
- Nut oils (almond, walnut)
- Chia seeds
- Hemp seeds and oil
- Flax seeds and oil
Dairy as if tolerable, aim for 2-3 servings per day
- Low fat plain Greek or regular yogurt
- Cheese (small amounts)
- Low fat cottage cheese
- Plant-based dairy alternative beverages and yogurts
Healthy snack options
- Apple slices with almond butter
- Carrots with hummus
- Guacamole with sliced bell peppers
- A piece of fruit or bowl of fresh berries
- Greek yogurt or cottage cheese with fresh fruit
- Hard-boiled egg with salt and pepper
Eat less of these foods with the Mediterranean diet
- Refined carbohydrates (white flour, sugar, soda)
- Saturated fat (butter, full fat dairy)
- Fried foods
- Red meat
Get started with healthy food swaps
You can start eating Mediterranean by swapping in foods that better align with this pattern for foods that don’t with your meals each day, and before you know it, it will become a healthy way of life.
- At breakfast as add some spinach to your eggs each morning with aside of whole wheat toast, or try oatmeal with fruit and nuts instead of pancakes
- For lunch as create a mixed greens salad with quinoa and chicken, dressed with a drizzle of olive oil, avocado and fresh herbs
- At dinner as roast seasonal vegetables to pair with grilled salmon and fresh fruit
Remember to drink plenty of water throughout the day (aim for half your body weight in ounces). And while red wine is an acceptable part of the Mediterranean diet (only one glass per day), we recommend considering imbibing less frequently.
The Mediterranean diet offers a no-nonsense way to nourish your body as well as protect your health for the long-term. And best of all, once you know the principles of the Mediterranean diet, you can modify your eating in a way that works for you, and focus on the foods you love.
Creating healthy eating habits can seem daunting. But don’t let that stop you. Access the expertise of our integrated care team who are specially trained to help you make lifestyle modifications that support your body in menopause. They will create a personalized wellness plan based upon your needs, as well as be your companion on following through.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
With all of the knowledge, self-awareness, and confidence that we gain as we age “about ourselves, our bodies, our turn ons and turn offs “ sex after 50 can be some the best sex of our lives. I know that can be hard to believe. We’ve all heard the negative messaging around menopause as the period of time when we lose our libido as well as our physical ability to enjoy sex. As a physical therapist who helps patients maintain their pelvic health, at every stage of life, I can tell you that it doesn’t have to be true for you.
Yes, menopause brings about significant changes as your ovaries stop producing estrogen. But, by focusing on your pelvic health, you can not only prevent and improve pelvic floor issues that put a damper on sex, you can also connect with your body in new and pleasurable ways.
Low Estrogen & Sexual Functioning
Several menopause-related changes can impact the way your body feels and functions during sex. As estrogen levels decrease, blood flow to the tissues of the vulva decreases, which can affect the size of the clitoris and its sensitivity to stimulation. The tissue of the vagina can become thinner and less flexible, and you may produce less natural lubrication which can lead to pain during sex. The same dryness that affects the tissues of the vagina can also affect the tissues in your mouth, which can make oral sex and even kissing a challenge.
These changes also tend to coincide with age-related muscle and sensory shifts, which can pose even more challenges to maintaining and enhancing one’s sex life. For many people, weakness in the muscles that surround the vagina, bladder and bowel can lead to urinary leakage, constipation, sexual dysfunction and pelvic organ prolapse. All of these things can contribute to how we feel about, and how we experience sex.
But changes in your body are nothing new. Through every menstrual cycle since puberty, your body has changed. If you were ever pregnant, your body has changed. If you’ve dealt with major illnesses or injuries, your body has changed. This is not to say that going through menopause is easy or to minimize the impact that these changes can have on your life, but you’ve experienced major physical changes before “ and both you and your body are incredibly resilient.
There’s clear evidence showing that addressing pelvic floor muscle function, in conjunction with improving overall muscle strength and physical wellbeing, can help to reduce and even prevent many of these symptoms related to menopause. Which brings me to the power of your pelvic floor.
Tap into the Power of Your Pelvic Floor
The pelvic floor refers to the multi-tasking group of muscles and connective tissues that make up the bottom of the pelvis. These muscles run from your pubic bone to your tailbone and wrap around the vaginal and anal openings. They also support and bring blood flow to the clitoris, vulva, and vaginal walls; and they are critical to maintaining and elevating your sexual function!
It’s important to keep all of your muscles strong and healthy as we age, and the pelvic floor muscles are no exception. During penetrative sex, the muscles that wrap around the anal and vaginal entrances, lengthen and open for pain free penetration and stretch, but they can also be squeezed for increased friction and sensation. Your pelvic floor is also important in orgasm with research showing that, during orgasm, the pelvic floor muscles will actually contract involuntarily.
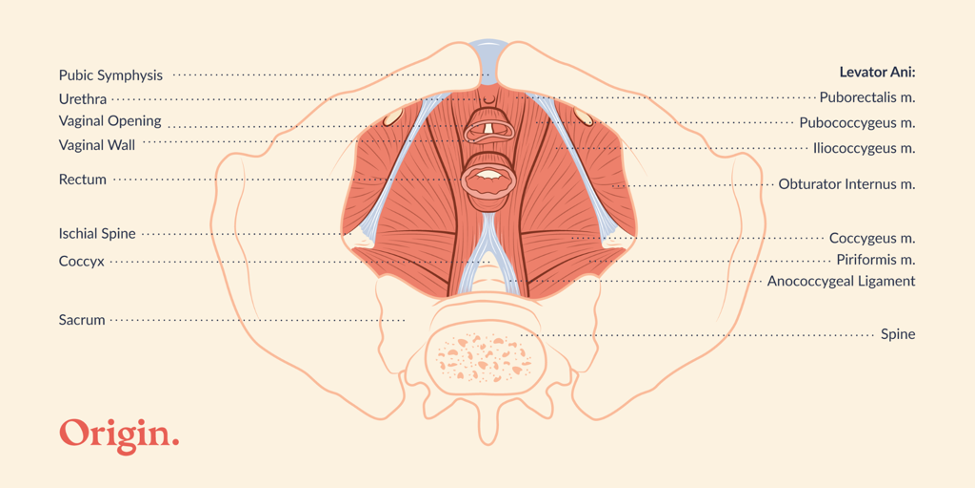
Strong, healthy muscles have better blood flow, and during arousal, your pelvic floor helps to prepare your genitals for sex by bringing blood flow into your tissues, helping with tissue engorgement, and increasing nervous system activity and sensitivity in all of your pelvic erogenous zones (your clitoris, labia, vagina, anus, cervix, and lower abdominals for example).
This is why one of the most physically important things you can do for your sex life is maintain your pelvic floor health. If you are unsure of where to start, try these tips below.
Make sex a habit. The “use it or lose it” principle is particularly important after menopause. While it’s not uncommon for sex frequency to slow down, it’s important to consider that if you aren’t having sex, or if it’s less frequent, the vagina may begin to narrow with less flexibility and increased atrophy of the tissues, which can lead to more pain and dysfunction during penetrative intercourse. If partnered sex isn’t an option or isn’t something that interests you, this is a great time for solo sex. Masturbation with a penetrative sex toy can be a great way to encourage blood flow to your vulvovaginal tissues.
Explore different kinds of touch. You may also choose to focus on outercourse, if your vaginal tissues feel pain during penetration. As your nervous system, and tissues of the pelvic floor change, what may have felt pleasurable before could start to feel irritating and unwanted. By focusing on touch and sexual activity that is pain free and pleasurable for you now, you can avoid taking part in the pain cycle that so commonly surfaces in menopause. Consider reaching out to a sex counselor, if you are looking for further guidance on how to explore different kinds of sex.
Maximize your pelvic floor muscle health. Even as we age, research shows that people who are sexually active and able to achieve orgasm tend to have healthier pelvic floor muscles. Since healthy pelvic floor muscles can encourage blood flow to where you need it most, you may consider learning strategies to improve your pelvic floor health, such as strengthening your pelvic floor or increasing the pain free flexibility of those muscles by using dilators or beginning a stretching program to address overactive and irritable muscles. It may even mean working on your ability to properly coordinate these muscles during sex.
To learn more about your pelvic floor and how it can improve your sex life, ask your gynecologist or primary care physician for a referral to a pelvic floor physical therapist. Your therapist will evaluate your pelvic floor muscle functioning and create a personalized treatment plan to address and prevent symptoms “ and help you feel good in your body right now, which may be the biggest sexual turn on of all.
Celestine Compton, PT, DPT is a doctor of physical therapy at Origin with a board-certified specialization in women’s and pelvic health. She continues to expand her knowledge and capabilities within the field of women’s health PT to provide her patients and community with the best care, advocate for her profession on local and national levels, and support the advancement of women’s health through contributions to research, public awareness, and education. As part of the Origin team, she hopes to do her part to raise the standard of care that all women receive at every stage of life and to improve patient access to quality care so that no individual, regardless of location, race, identity, education, sexuality, or economic status is left behind.
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
“
Menopause information and advice is available everywhere now, and literally at your fingertips. And with a quick search with Doctor Google, you could either find some very valuable resources, or be taken down a path of misinformation. Gaining reliable advice as well as evidence-based treatments to manage your symptoms is what we are all about here at Gennev. So, we tapped into Dr. Lisa Savage, board-certified OB/GYN, to answer questions from our community about menopause, and help dispel the myths and share the facts surrounding symptoms and treatments.
Will my migraines disappear after menopause?
Headaches are very common, and what happens during menopause is highly variable. I’ve had plenty of patients whose migraine headaches do get better, others who got worse and many who stayed exactly the same. It’s not predictable and it’s very individual.
Some women have a cyclic component to their headaches (menstrual headaches) that come on as a prelude to menstruation, and lift after your period is over. Those types of cyclic headaches generally get better with menopause when cyclic hormones are not playing a role. Ultimately, I think it probably takes about a year after that last menstrual period to really know where your headaches have ended up – and even after that, there may be some change that can go either way.
How long does it take to feel better on HRT?
Time to symptom relief is a really gratifying part of starting HRT because it doesn’t take long. It’s not delayed gratification. I always tell my patients I don’t want to overpromise, but typically results can be seen anywhere from 48 hours to a couple of weeks.
How long can you take HRT?
It’s very individualized, and it depends on how old you are, when you need to start, and how long you want to take it. HRT does not need to be a long-term commitment if you don’t want it to be. Some women will take it for a few years to relieve the worst of the symptoms, and some women will need it longer, especially if they started their menopause transition at a younger age. Usually when a woman is approaching 60, I’m looking to see if we can get her off HRT, assuming she was around average age for menopause”¦meaning she’s been on it for around 10 years. I like to describe the therapy goal as extracting the most benefit while minimizing risk. But again, it’s not written in stone and there’s no hard and fast stopping point. Some women have ongoing symptoms for which they need the HRT. The most recent NAMS statement on HRT has taken away some of the boundaries about duration of treatment, which allows for our favorite way to prescribe medication; that is, with a lot of individualization.
Should I fear using HRT because it can cause breast cancer?
The short answer is no, but the better answer is “it depends.” There’s no doubt that some susceptible women, such as those with certain family history or genetic risk factors, may not be able to or want to take HRT because it may fertilize a propensity to develop breast cancer. It’s true that with longer term use from combined (that is estrogen and progesterone”¦not estrogen alone) HRT, there’s a small increased incidence of breast cancer. It’s about 8 extra cases per 10,000 women, so the absolute risk is very low. The increased risk from two glasses of wine per night or eating red meat is higher, to put it in perspective. You do have to commit to screening mammograms and knowing your body. I put this in terms of risk benefit ratio more than cause and effect. So often the benefits are going to outweigh any potential risk. We consider the individual patient and her individual profile when it comes to HRT.
Can women start having migraines in perimenopause if they’ve never had them before?
I’ve seen women start having migraines in perimenopause, but headaches are so multifactorial, especially vascular headaches. And my sense is that the sleep disturbance that comes along with perimenopause transition may play a big role in headaches. We all know if we’ve had a restless night’s sleep, the next day we don’t feel as well in our body. Maybe more headachy. I believe there’s a real sleep disturbance component to these headaches.
If you are post-hysterectomy, do you need to take the progesterone with the estrogen?
The only job of the progesterone in HRT is to protect the uterus from overgrowth of the lining. So, if a woman does not have a uterus, whether or not she still has ovaries, then she doesn’t need a progesterone. There’s some evidence to show that the combination of the estrogen plus the progesterone (the E + P) is what can cause some additional risk over time.
Is there a connection between autoimmune diseases and menopause?
Autoimmune is highly prevalent in women compared to men, and estrogen plays a role in autoimmune disorders and immunity in general. But immunity is also influenced by genetics, lifestyle and environment, so it’s hard to carve out just the estrogen component. It definitely plays a role in some autoimmune disorders such as rheumatoid arthritis and MS as as they may get worse with menopause. Lupus sufferers may actually feel better with menopause. But this varies greatly as it’s based upon the individual patient.
Is it true that the earlier a woman starts puberty, the earlier they’ll start menopause?
Not necessarily. A lot of women think if they were a late bloomer, they will not go through menopause until later. Or perhaps they started their periods when they were ten years old, and think they’re going to finish earlier. These things are not necessarily correlated. The average age of menopause across the board is 51. The normal age range is 45 to 55, and it’s independent of how old a woman was when she started puberty. Family history may actually be helpful; that is, knowing how old your mother or older sisters were at the time of menopause may be somewhat predictive.
Should I worry if I’m 59 and haven’t hit menopause yet?
This is definitely older than average (by the age of 55, 95% of women have completed the menopause transition), but as long as you’ve been getting medical care from a clinician who is familiar with these things and there is good confidence based on menstrual history and (in this case) labwork, that you are still pre-menopausal and not having post-menopausal bleeding, there are benefits to ongoing ovarian hormone production. There is a silver lining there for your bones, cognition and cardiac health.
Is weight gain a side effect of HRT?
No, HRT does not cause weight gain. But it is true that many women start HRT coincident with the onset of menopause, which does bring metabolic changes. Increased weight around your midsection is very common at this stage of life, even if you have never had it before. It’s the body’s way of compensating for the loss of ovarian estrogen production, since estrogen can also be made in fat. To a certain point (say 5-10 pounds), I usually encourage patients to be accepting of a new normal and not too go crazy trying to maintain a weight that they were five or ten years ago. Some changes in nutrition can be helpful, along with getting adequate sleep, and exercise.
What can I do about hair loss or hair thinning with menopause?
It is true that aging in both men and women can cause hair to thin. I never automatically attribute this to menopause and always encourage patients to see their dermatologist. Thyroid disorders, among a list of other things, can cause hair loss. Depending on the pattern of hair loss on a physical exam, labs and/or scalp biopsy might be indicated. Menopause absolutely can contribute to hair changes, but please see your dermatologist for an examination, blood work and investigation before assuming it’s strictly based on menopause.
Does HRT prolong menopause?
HRT does not extend or prolong menopause. This is a common concern among women considering HRT. Menopause symptoms tend to dissipate over time naturally, and so your symptoms are going to be what they are at that age, whether or not you took any HRT.
Is there a certain age that someone is going to start menopause?
It’s highly variable. I always say 45 to 55, but a lot of women will start to notice changes in their late 30s and I call those prelude symptoms. This is when symptoms tend to come and go. Certainly, into your mid 40s it is very common to start seeing some symptoms, even if they’re not consistent.
Is a woman infertile because her periods have become irregular?
You may still ovulate from time to time until you have gone a year without a period. So even if your period is not regular and predictable, I always tell my patients they still need contraception until they’ve been a year without a period. Irregular periods are not a form of birth control.
Is more painful ovulation a sign or symptom of perimenopause?
It doesn’t seem fair that when we’re trying to end our reproductive years that we have to get more pain with it. But I’ve seen many patients that report more painful ovulation and periods, and more PMS during perimenopause compared with the earlier years of their reproductive life.
If my hormone labs are normal then I’m not in menopause or perimenopause, right?
Not necessarily. Labs indicate levels in a snapshot – a moment in time as and they may vary a lot from one day to the next. If we look at a woman at the right age with classic symptoms, the labs might still be normal, or they may be normal today and not tomorrow. So, it’s good to not to rely on them, as normal labs may not mean that it’s not perimenopause.
What are your tips for relieving increased PMS during perimenopause?
There are a lot of holistic things I go back to like exercise, eating well, and adequate sleep. I have prescribed very low dose birth control pills for women in perimenopause who have a lot of PMS as women who do not ovulate do not have a lot of PMS symptoms. The pill eliminates ovulation so that that can be a nice transitional thing to do.
How do you feel about testosterone pellets as hormone treatment?
I don’t use them. Testosterone is typically prescribed for libido, and in order to make a difference on that, you have to use really high doses of testosterone. I call that trying to make a woman into a man – and there may be some cardiac risk associated with that. So, I am not a believer in the use of testosterone for women. Other doctors disagree, and I respect that, but I’m not a fan of testosterone in any form, whether it’s pellets or creams, patches, etc., and I’ve not found it to be helpful.
If you are in menopause, should you avoid regular Pap smears or have them more frequently?
Menopause really doesn’t influence our Pap recommendations for most women over the age of about 30. If you’ve had normal Paps, you can get one about every third annual. There are some age-based recommendations on how often to get a Pap, but typically we’re going to do Paps up to the age of about 65, assuming normal results over time. Menopause doesn’t influence whether or not to get a Pap smear.
Will all this extra protein in my diet make me fat?
I always promote a diet consisting of lean protein and vegetables, more specifically the Mediterranean way of eating. I think we really have to watch out for the carbs and especially refined sugars. As we age, we’re losing muscle, and estrogen does play a role in maintaining lean muscle mass. So, when your estrogen is decreasing and your muscle mass is naturally decreasing, having that additional protein can help to rebuild, repair, and maintain that muscle.
Are low dose antidepressants effective for hot flashes?
Yes, I’ve had some good luck with this. Especially for patients who cannot take hormone replacement therapy, or don’t want to. We know that certain low dose antidepressants can help with hot flashes. Additionally, menopause frequently brings mood disorders. It can unmask depression and anxiety or make it worse. So, you may get some double coverage by using a low dose antidepressant for hot flashes and moods. But I will say that as helpful as they may be, there’s nothing as effective as estrogen for relieving hot flashes.
What is your trusted advice for women going through menopause?
I always say be aware of “Doctor Google”. Getting your information from Doctor Google can be like drinking out of a firehose and you don’t know what’s reliable and what’s not. Rely on your physician, and specifically in menopause, your OB/GYN physician. Narrow your resources to reliable ones such as gennev.com, acog.org and menopause.org.
You can listen to the “Menopause Myths & Facts” interview with Dr. Savage here.
We can help relieve your menopause symptoms
You deserve the support, education and specialized menopause care that will help you start feeling better now. Learn more about Gennev’s Integrated Menopause Care by clicking here.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
The changes women experience during menopause don’t just affect their insides. Skin and hair also go through a transition. If you’re seeing noticeable changes in the health, texture and appearance of your hair and skin, chances are you can blame declining levels of the hormone estrogen. These unwanted and often unexpected changes can be frustrating, but there are things you can do to protect your skin and hair throughout the menopause transition.
Since estrogen is linked to hair growth, density and fullness, as hormone levels decrease, head hair can become dryer, more brittle, and thinner. And due to a greater proportion of androgens (male hormones), you may begin to notice some hair on your face that’s more like male facial hair, particularly on the jaw line. You may also notice a decrease in body hair, including the pubic area.
Declining estrogen also means skin gets thinner and less elastic due to a decrease in collagen. Without their usual supply of estrogen, our bodies produce less of the oil that both softens skin and helps it retain moisture. Menopausal skin loses elasticity and hydration and becomes thinner, dryer, and loose. Many women find they have acne again for the first time since puberty. Skin becomes more prone to rashes and bruising and may heal more slowly during this time.
There are many causes for changes in hair and skin as you age. It’s best to visit with a dermatologist for diagnosis and treatment, as well as to rule out any underlying conditions that may be attributed to what you are experiencing.
Medical interventions for unwanted menopausal hair
If you are dealing with unwanted facial hair in menopause, there are a few options to consider, although they can come with some downside:
- Topical treatments as these can be expensive and require continued use or the hair grows back.
- Depilatory creams can be bought over the counter, but they may be a bit stringent for the face, particularly as skin gets more sensitive with age.
- Lasers shoot beams of light over the skin, overheating the hair follicles and destroying them so the hair doesn’t regrow, but this can take several treatments to become permanent, and it doesn’t work on fine or light-colored hairs.
- Zapping hair with electrical current in electrolysis is expensive and slow because it can only destroy one hair at a time. It’s permanent, but can take a long time to complete, hurts, and can potentially scar.
Medical interventions for hair loss
The signs of hair loss in women may include an increase in hair falling out each day, noticing patches of thinner or missing hair, a widening part at the top of your head, or even noticeably smaller ponytails.
Before pursuing hair loss treatment, it’s important to talk with your doctor or dermatologist to learn the cause of your hair loss, as well as treatment options that are right for you . Your healthcare provider will do a thorough history as well as order relevant tests to help diagnose your hair loss:
- Blood tests to evaluate ferritin levels, vitamin and mineral levels
- Blood tests to evaluate hormone levels including your thyroid and sex hormones
- Scalp biopsy or Trichoscopy (non-invasive dermoscopic imaging of hair and scalp)
- Hair pull – doctor gently pulls on your hair to see how many hairs come out
If it’s thinning head hair you are experiencing, unfortunately, there are few solutions. The good news is, the loss generally slows as hormones level out.
- Minoxidil (Rogaine) can help you regrow some hair, though you have to keep using it. “
- Anti-androgens may work for some women for whom Minoxidil is a non-starter.
- For some women, an iron deficiency may be partly responsible, so an iron supplement can be helpful. Be sure to consult with your doctor before starting any new supplement regimen.
- Hair transplants have come a long way since hair plugs and can be quite effective in filling in patches where hair has thinned.
Medical interventions for changing skin
Before you do anything to aid your age-related skin changes, we recommend locating a dermatologist who has experience with women in menopause, as all skin is different and should be treated with real care. Note that some procedures work best on skin that’s aged from sunlight rather from estrogen loss. Some options include:
- Prescription-level retinoid skin creams, made from vitamin A extract.
- “Peptide creams use amino acids (though these are likely less effective than retinoids).
- “Microdermabrasion encourages new skin growth by removing the top layeras it is time consuming and expensive and the effects only last about 4 weeks.
- “Laser resurfacing of the skin uses high-intensity light to tighten loose skin, improving the look of wrinkles.
- Newer non-ablative laser resurfacing doesn’t cause wounds to the skin, so recovery is quicker. The heat generated by the laser promotes collagen production which causes the skin to tighten and look younger and healthy.“
- Chemical peels remove the upper layer of the skin and encourage new growth.
Lifestyle modifications for healthy skin and hair
Probably the best thing you can do for your skin and hair, no matter what your age, is protect what you have.
- Reduce sun exposure, and use SPF every day.
- Use gentle products that don’t strip away the remaining moisture.
- Hydration is key. Drink plenty of good, nutritious water to hydrate your body from the inside out.
- Don’t smoke.
- Shower with cooler water for less drying of your skin.
- Moisturize skin and condition hair. Replacing the moisture you’ve lost isn’t entirely possible, but every bit helps.
When it comes to skin, we strongly advise getting to know your skin very well. Checking your skin every month for changes can perhaps mean catching a potentially serious problem like skin cancer while still in its early and more treatable stages.
Natural remedies for skin and hair
For unwanted facial hair, sugaring, tweezing, waxing, and threading may be slow and tedious, but they can be less expensive, less potentially damaging to skin, and reasonably effective, if a bit painful.
To preserve head hair, use gentle styling techniques that require less heat and pulling. Shampoo with zinc or selenium might help with a dry and itchy scalp. A shorter hair style might help make hair appear fuller.
Some say eating estrogenic foods such as soy, dried fruits, and flaxseed can help, though there’s no research to back that up. Others take collagen supplements, though currently there’s little evidence to prove the impact on menopausal hair and skin.
The effect of changing hormones on your hair and skin may seem out of your control, but when you prioritize your wellness during this stage of life, you will support your body and your beauty from the inside out. Keep feeling and looking your best in menopause and beyond by maximizing your nutrition with a healthy and balanced diet, staying hydrated as well as exercising each day. And please visit with your doctor or a dermatologist when it comes to concerning hair and skin changes, no matter what your age.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Many women in menopause find their standard eat-and-exercise routine no longer works for maintaining weight. The reality is, in menopause, you’ve probably lost some muscle mass, and with it the higher metabolism that burns more calories faster. On average, midlife women gain 1.5 pounds (0.7 kg) per year. Managing your weight in menopause is simply more difficult.
Metabolism and weight gain in menopause
Body fat produces estrogen, so a little extra of the former means more of the latter to ease your transition and help protect your bones, brain, and heart. That said, menopause also directs your body to put more of the excess weight on your belly, rather than it landing on your hips, thighs, and buttocks, as it did in your reproductive years. Belly fat is more problematic, because it can contribute to heart disease and metabolic syndrome. So, if you find you’re gaining more than you’re comfortable with, there are things you can do to re-rev metabolism and maintain a healthy weight.
A smart first step we always recommend is talking with a doctor or a Registered Dietitian to find out what is truly a healthy weight for you. Talk about any risk factors you have for exercise and ask if any of your medications may be contributing to weight gain and could be safely swapped out for another without that side effect. Generally, doctors won’t prescribe medications or procedures for moderate weight gain, as better lifestyle choices and acceptance of your post-menopausal body are the healthiest paths (hard as we know those can be!) A weight gain of 10-15 pounds during the menopause transition is typical. And if you are lean going into post-menopause, weight gain may actually be protective.
Lifestyle modifications for weight management
At this stage of life, your body requires fewer calories to function – so if you eat the same amount that you did in pre-menopause, you’re likely to gain weight. Also, perimenopause can suppress leptin (the satiety hormone), and ramp up ghrelin (the hunger hormone), making you feel hungrier. We’ve rounded up the eight lifestyle changes that have proven effective in supporting weight management for the Gennev community.
Embrace your changing body. The biggest lifestyle tip we suggest is to embrace and accept your changing body. It may be a little softer and rounder in spots, and that’s perfectly normal and OK. It’s important to first focus on health. Looking good is great; feeling good is even better.
Optimize your diet. Obviously, this is a biggie. Now is the time to really pay attention to nutrients first and foremost to support brain, bone, and heart health in the years ahead. Fortunately, good food and beverage choices for those tend also to be good choices for minimizing menopause symptoms, including weight gain. Not so much a “diet” as an eating pattern, the Mediterranean diet is the most healthful for women in menopause. It focuses on lots of veggies, plus fruits, whole grains and lean proteins. This style emphasizes eating things closer to their natural state (minimally processed) for the highest nutrient density and ease/efficiency of absorption.
The DASH diet has similar advantages to your body; in fact, it was devised specifically to help treat or prevent hypertension. In addition to many of the same foods advocated under the Mediterranean diet, DASH also advocates limiting salt. Protein, healthy fats, and fiber are how your body reaches satiation and stays there longer, so be sure you include enough of each.
Food journaling. If you eat the same amount that you did in pre-menopause, you’re likely to gain weight. When we’re stressed or our hormones are doing strange things, it can be difficult to have a real idea of what we’ve consumed during a day. Keeping a journal helps us get a clearer picture of our eating (and snacking) habits. BONUS: Journaling may also be a way to uncover food sensitivities that didn’t exist previously and that cause other issues like gas or inflammation.
Hydration. Believe it or not, what we think is hunger is often dehydration. Remember, you should be drinking half your body weight (in ounces) every day, so before you have a snack or seconds, drink some water and see if you’re still hungry. If you are, eat! Hydration is so good for us, and you may need more of it if you’re dealing with night sweats and hot flashes.
Sleep. There is a very strong association between not getting enough sleep and weight gain. And yes, sleep is a bear to get during perimenopause and menopause, so do the very best you can to practice smart sleep hygiene and maximize your chances of a good night’s sleep.
Exercise. Even if you’ve been a dedicated exerciser, you may find that your usual routine no longer has the effects it once did when it comes to controlling weight. Changing up the balance of cardio vs strength training can help in lots of ways, to help you manage weight, sleep better, manage stress, and put some healthy demands on your bones. It’s important to keep moving in menopause and beyond for both the emotional as well as physical health benefits.
Mindfulness. “Mindfulness” is the art and science of being fully present and in the moment, and when it applies to eating, it can really help you eat better and less. Being mindful when menu planning and grocery shopping adds to the bounty of goodness this practice delivers because you won’t get home to discover some bags of empty calories, salt, sugar, chemicals, and saturated fat mysteriously ended up in your cart. Mindful eating means not doing other things while eating” no TV, no Internet, no phone calls or emails. Instead, be aware of the now:the smell of your food, the colors, the sizzle of heat, the shine of glaze. As you eat, note not just the taste but the mouthfeel and texture. Try to experience the component flavors: is there a hint of thyme? The more aware you are, the slower you’ll eat and the better you’ll recognize when you’re satiated.
Try Green Tea. Green tea has helped many women with menopause symptoms, including weight gain. Possibly the catechins in green tea accelerate metabolism ever-so-slightly or boost the burning of calories. There isn’t sufficient research to say how or even if green tea works its magic, but it might be worth adding a cup to the early half of your day (it’s caffeinated, so maybe drink before noon and stick to no more than one or two cups per day).
If weight gain continues to trouble you, it’s important to speak with your doctor before it becomes a serious health risk. They can advise of medical interventions that may be right for you based upon your individual weight management goals.
Menopause, body weight and shape changes
Gennev recognizes that the body weight and shape changes which occur with aging and the menopause transition often leave women feeling uncomfortable in their bodies and concerned for their long-term health. Based on current research we know diets work, but with caveats. Most diets leave most women feeling deprived and frustrated to only gain back the weight they lost (and sometimes more). Through our team’s experience working with countless women and accounting for the physiological and metabolic changes that occur during menopause, we have developed the following approach to address these three important components.
Start with YOU – understanding you as the individual, your place in the menopause transition, your current habits, concerns, and goals is our starting point. Our Integrated Care team meets you where you are and supports you along the way to feeling better in your body:
- Assess current and past nutrition habits and relationship with food and body
- Listen to your health worries and questions
- Account for your lifestyle, resources, time, and energy available
- Address where you are in the menopause transition and the influence that has on recommendations
Cater to menopause physiology – the changing hormones during peri and post menopause result in a physiological and metabolic state which is different from pre-menopause. Strategies that work with rather than against these changes offer greater benefit and long-term sustainability. They include:
- Meeting protein needs
- Assessing carbohydrate intake and adjusting to account for blood sugar response
- Incorporating anti-inflammatory foods/Mediterranean-style nutrition
- Movement that feels good (and ideally includes resistance training)
- Rest/recovery/rejuvenation/mobility
Activate the Gennev menopause mindset – a proprietary combination of cognitive behavioral therapy, abundance mindset, and motivational interviewing that supports women in embracing what can be rather than wishing for what was.
- Empower with knowledge
- Self-compassion
- Mindful/intuitive eating
- Living forward with more peace and confidence, and less resistance
With this approach some women will lose weight, and some women will find that they are exactly where they are supposed to be. All women will gain the health benefits of implementing habits supportive of metabolic and physical health as this stage of life.
We understand how frustrating it feels to not get the results you want when you have been working so hard. We invite you to try a different approach and learn how Gennev’s Integrated Care Team can support you with your weight loss goals.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
“
Perimenopause (the time leading up to menopause) typically begins for women sometime in their 40s. This is when you may begin noticing menopause symptoms including hot flashes, interrupted sleep, lower energy, and mood swings. And as women arrive at menopause (defined as when a woman has gone 12 consecutive months without a period), they may also be affect by a slowing metabolism. Menopause brings with it many bodily changes, but a well-balanced diet and nutrition can help support you on your journey.
Through the menopause transition, hormones (primarily estrogen and progesterone) are fluctuating as they slowly decline. These changes create a new physiological environment for the body which has metabolic effects that influence how the body metabolizes food. Consuming a well-balanced diet is key for optimizing health throughout all stages of life, but during menopause it becomes even more important.
“The changing hormones of the menopause transition create stress on the body, albeit a normal natural stress, it is stress nonetheless. Being intentional about optimizing your nutrition during this time can support your body through managing the stress of the hormone changes. By giving your body this support, a reduction in symptoms can occur in the short-term and overall health can be supported in the long-term.” –Stasi Kasianchuk, Registered Dietitian Nutritionist, Exercise Physiologist, and Certified Specialist in Sports Dietetics
Key nutrition recommendations for menopause
Stasi Kasianchuk, a Registered Dietitian Nutritionist, and Gennev’s Senior Director of Lifestyle Care, shared with us key nutrition recommendations for women in menopause that will support the body through the transition and optimize health outcomes now and into the future. Stasi suggests that first, it’s necessary to examine our relationship with food. “At times in our life when our bodies change in ways that feel outside of our control it can be tempting to see food as the enemy and want to restrict or limit your intake.” Stasi recommends, “During the menopause transition, when your body is already managing the stress of changing hormones, restricting calories can further exacerbate the stress response resulting in undesirable consequences. Establishing a positive relationship with food by focusing on nourishment and support, can be helpful to get the most out of the following recommendations.”
Rather than low carb or no carb, focus on strategic carb. Estrogen influences carbohydrate metabolism, so as estrogen levels change during the menopause transition, so does the way the body uses carbohydrates. The body’s ability to respond to insulin secreted in response to carbohydrates consumed also decreases and can lead to increased blood sugar levels. This does not mean you need to eliminate all carbohydrates, in fact that will have the opposite effect and typically exacerbates undesirable blood sugar spikes. Strategically approaching your carbohydrate intake, with the majority of these coming from fruits, vegetables, and wholegrain sources, can help to meet your carbohydrate needs and support an optimal blood sugar response. Refined or simple carbohydrates can certainly be enjoyed, as this is part of having a positive relationship with food, and also make a great fuel source prior to exercise, especially high intensity training.
Prioritize protein. Most women are not aware that protein needs increase during peri- and post-menopause. Having adequate protein from food is important to provide the body with the building blocks to support muscle mass which naturally declines during this phase of life. Aiming for 20-25g of protein with each meal and especially after resistance training and high intensity interval training (HIIT) can help to mitigate muscle loss. While all foods containing protein are beneficial, protein foods which contain the amino acid leucine are particularly helpful for stimulating muscle growth. These foods include eggs, beans, legumes, chicken, salmon, brown rice, and chia seeds.
Fats are your friend. The hormonal shifts during peri- and post-menopause allow the body to better utilize fatty acids. The key here is to prioritize fats from unsaturated sources, especially those containing omega-3s such as salmon, sardines, walnuts, and flax, hemp, and chia seeds. These support brain and heart health and help the body manage inflammation.
Think in color. Focusing on eating a variety of colorful foods typically results in eating more fruits and vegetables which offer fiber and nutrients to help the body better manage inflammation which can increase with the changes in estrogen and progesterone. The hormonal changes during peri- and post-menopause can also influence the gut microbiome. Women may experience changes in digestion as a result. Supporting the gut with a variety of plant sources of fiber not only supports optimal digestion, but also promotes satiety, helps lower levels of blood cholesterol, and stabilizes blood sugar, all of which are also altered when hormone levels start to shift.
Bone support. While dairy foods can certainly support bone health, they aren’t the only foods that provide bone building nutrients at a time when bone formation is no longer occurring. A combination of foods containing calcium, vitamin K, magnesium, vitamin D, and protein synergistically can support maintaining bone. These foods include dairy products, tofu, nuts, seeds, leafy greens, and plant and animal sources of protein. If you have limited exposure to the sun, you may benefit from supplementing with at least 2000 IU of vitamin D per day (check with your doctor to confirm your needs).
Take note of symptom exacerbators. Perimenopausal symptoms such as hot flashes, night sweats, sleep disturbances, anxiety, and mood swings are some of the symptoms that can be exacerbated by certain foods. These include refined carbohydrates/simple sugars, caffeine, and alcohol. Pay attention to your symptoms when you consume these foods or beverages. If you notice your symptoms getting worse it doesn’t mean you have to eliminate these items, but a modification to your intake may help you to feel better.
Implementing these nutritional strategies along with making time for daily physical activity will not only help relieve symptoms, but will support your overall health throughout the menopause transition and beyond. If you need additional guidance in developing a healthy diet in this stage of life, our menopause specialists can be a great resource for creating a personalized plan that supports your body’s changing nutritional needs, relieves symptoms, and optimizes your health for the long term.
“
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.