If her name looks familiar, it’s because Dr. Meagan Peeters-Gebler PT, DPT, CSCS, CMTPT, along with colleague Dr. Brianna Droessler-Aschliman PT, DPT, CMTPT, have been doing a monthly blog with Gennev for several years.
They’ve educated us on pelvic floor issues such as incontinence, prolapse, and sexual function; they’ve taught us about high heels and standing desks; helped us understand and relieve pain and keep our bones strong.
In this video/podcast, Dr. Meagan speaks with Gennev Health Coach Stasi Kasianchuk about pelvic function. What are the pelvic muscles? What do we use them for? How do we keep them strong and fit?
Watch the video of Pelvic health with Dr. Meagan Peeters-Gebler on YouTube. Full transcript is below.
The Path To Better Pelvic Health
Gennev:
Welcome to the Gennev podcast. In this series we talk with the experts about women’s lives and health in menopause. Our mission is to empower you with information that puts you in control of your health. We’re glad you’ve joined us. Let’s get started.
Coach Stasi Kasianchuk:
Today, like we talked about, I want to get your insight as a Doctor of Physical Therapy on pelvic health, pelvic stability. I’ll start off by introducing myself to our audience. So I’m Stasi Kasianchuk, I’m a Gennev menopause coach and I’m also a registered dietitian nutritionist with expertise in sports nutrition and exercise physiology. So with this topic I’ll start it off by saying I have a, I’ll call it somewhat understanding of pelvic health. I know it’s important from my anatomy and physiology classes and previous life as a group exercise instructor and personal trainer. I’m familiar with that musculature, but I know now that there’s been a lot more research and a lot more targeted approaches for pelvic health and stability. And so I’d love for you to just introduce yourself, your role as a Doctor of Physical Therapy, maybe give some insight into what that is in case some of our audience members are not sure of it. And then what is your role specifically in supporting women’s health?
Dr. Meagan Peeters-Gebler:
All right, thank you. My name is Meagan Peeters-Gebler and I am a Doctor of Physical Therapy as well as a postpartum and pregnancy corrective exercise specialist and a certified strength and conditioning specialist. So you know, as a Doctor of Physical Therapy, our introductory education is, is pretty general into the field of women’s health and pelvic health. So most of us who go on to pursue this specific area of study, it’s kind of postgraduate work and continuing education to acquire those skills and knowledge. And it is basically looking at the pelvis as a part of the whole, right. So you know, kind of as, as general PTs, we often look over the fact that it’s muscles, tendons, ligaments, nerves, bones. It is made up of exactly the same stuff that our necks and our backs and our shoulders are. And, and just making sure that we recognize its important role in the musculoskeletal system for pain, and like you alluded to for lumbopelvic stability but then also for continence or keeping, keeping our urine and stool in, and then sexuality. So I’m kind of putting all those pieces together and figuring out how mechanically as PTs we can promote better overall health and function to those, those areas.
Coach Stasi:
Excellent. That’s a great overview and gives us some good things to talk about and to dive deeper in. I would say so as an exercise physiologist and like I said, previous personal trainer and someone that also tries to make exercise a part of my life, in a way, honestly, my goals really are to stay healthy and to have longevity and understanding the learning more about the importance of musculature all over our body and pelvic health has really, as I’ve been in this field a little bit longer, learning more about that. So my general understanding is that the pelvic floor as you plays a role in obviously continence and making sure that urine and stool do stay where they’re supposed to be until we actually move them out on our own planning versus not. And then also from a core stabilization, I mean the pelvis is really close to the low back. It’s the connection to a lower body. So I’ve had an understanding that that strength in that area can also be important for decreasing risk of injury in other areas of the body. I would love for you to just dive into that. Correct me if I’m wrong on some things. And you know, let’s clarify some of this for our listeners.
Dr. Meagan:
Definitely. So I always like to point out that, you know, research has shown that disorders with continence and breathing actually have a higher correlation to low back pain then obesity or inactivity. So I think that is kind of a, a profound, you know, like way of, of really recognizing the importance of the pelvic floor, but then also the respiratory diaphragm as it relates to the pelvic floor in kind of a systemic container pressure management system. Right. We know that, that the pelvic floor, yes, is, is kind of a hammock of muscles that slings across the bottom of the pelvis.
Coach Stasi:
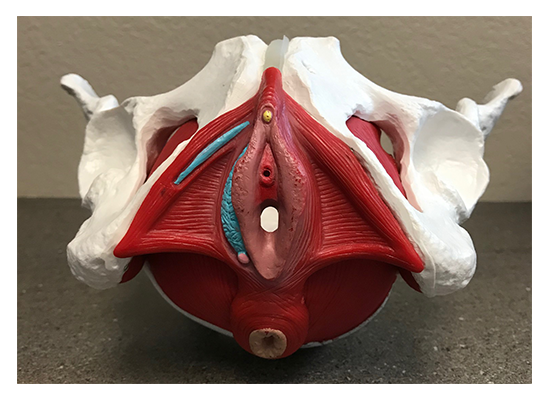
A visual!
Dr. Meagan:
Yeah. So it’s there, it attaches to, you know, the entire pelvis, it attaches to the tailbone and the sacrum. And it really does span and serve as like a structure and a structure to that the whole bottom opening of, of our body. And, and if there’s either weakness or incoordination, there is going to be an inherent vulnerability to everything that is stacked on top of that.
Coach Stasi:
Oh, that’s such a good point. Yeah. And is it possible? I guess what I notice a lot with a lot of the clients I work with through the HealthFix Program is that all of a sudden during menopause, things are just happening all over the place. And, they start to notice things that they may have not noticed before. So, you know, related to pelvic health, maybe all of a sudden there is more incontinence or they’re really wanting to improve sexual function or get their sexual function back. Is it possible, over time because someone may not be aware of this, we may not be working on supporting our pelvic health, then menopause hits with all these other things. And it’s accumulation of not supporting pelvic stability for years that happens at this point? Or is it really something that during menopause, the decrease in estrogen and what’s going on during menopause affects?
Dr. Meagan:
Yeah. You know, I almost so clinically I see it. Plus it’s like the straw that breaks the camel’s back, right: So, you know, gravity and bad habits and posture and life have been like cumulating insults on these poor structures. You know, we also know that the vast majority of women who are verbally taught Kegels are doing them wrong. So so it’s, it’s almost like, yes, we’ve been exposed to all of these challenges. If we’re even worse patients, you know, with without estrogen and without that good blood flow, suddenly these healthy, plump muscles get thin, and fragile and weak, and just the structural integrity automatically diminishes if you do nothing else besides ride it out. So, so wanting, wanting to either prepare before, be actively engaged during and, and figure out continued maintenance from a PT perspective I think is huge to navigate that time.
Coach Stasi:
Yeah, and I would say some of the questions that I get from a lot of the clients I work with, a lot of them are having back pain or knee pain. Are some things there. And I often recommend that they do exercises with a physical therapist, go to see a physical therapist to make sure that they’re doing exercises correctly. And you bring up a good point about the Kegels that most people are doing them wrong. So can you talk a little bit about what you see as maybe some challenges for women and then how you address that? And maybe give us some instructions on what is the correct way to do Kegels, if that’s possible over a podcast.
Dr. Meagan:
Right. Yeah, definitely. So you know, I think what, what we encounter typically in a clinic is that, kind of two diverging paths. One is that women are either squeezing with all their might, kind of everything between their ears and their eyebrows and their knees and their toes, like everything is gripping. And that is just too much that they end up actually generating too much pressure and making their pelvic floor have to work too hard.
And on the flip side, it’s that there’s absolutely no connection. You know, it’s like pelvic floor, what? Is that my anus, is that my, you know, like how do I even feel that, like I don’t feel anything moving. So it’s that women are either excessively connected or totally disconnected to those parts of the body. Usually what we do is we kind of take the approach of helping them find those body parts at the base of their pelvis through the breath. Because when we use the breath, what we can do is we end up tapping into some of the automatic reflexes and just exploiting the physics of how pressure moves through your body as a container to help them hone in on exactly what parts they should be feeling, in which direction, and to what extent.
Coach Stasi:
Oh, interesting. Is that something you could even direct me through right now over the over the podcast? I’ll give it a trial, like, you know what I’m feeling?
Dr. Meagan:
Yeah. So, so kind of the spiel that I like to give is that our body is a container, right? We have air on top in our lungs and in our rib cage. Then we have a diaphragm that separates our air from our guts, then we have our guts. And then we have our pelvic floor, right? And as air moves through our container, the shape of our container should change. And the pressures inside should also change. So as you inhale and you inflate your container, your rib cage should expand in all directions to accommodate that, that added air. Your diaphragm should drop to make more space for air. And in doing so, your guts should bulge out to the front and down to the bottom a little.
So on an inhale you should feel your perineum, your pelvic floor, kind of that space between the vaginal opening and the rectum and the anus drop slightly in response to the fact that air has been added to the system. Okay. On the flip side, when you go to let the air out and exhale, which you’re going to feel is your rib cage shrinks, your diaphragm actually lifts up kind of following the air out of your body. That creates a loop, a little vacuum that pulls your guts up and in as well as your pelvic floor. So we like to get gals kind of rocking and rolling with that breathing rhythm where on the inhale inflate, notice the pressure in the expansion. And then on the exhale, think about gently lifting two beans, right? So think about squeezing around and pulling up and in at the vaginal opening as well as at the anus.
And you want to include, well the front and the back openings because the pelvic floor muscles sling around both of them. Yes. Okay. So you inhale, inflate, feel things descend and then you exhale, lift, gently squeeze and notice that there’s a lifting action that happens.
Coach Stasi:
Wow, that’s incredible. I don’t, I think I’ve ever thought that process through and it’s a good reminder of really that deep belly breath versus the short inhalations that we… myself, I’ll speak for myself to have a tendency to do more often where that is such a valuable benefit. And I actually, I have never heard of that comparison before, so that was really helpful to take that time to really think about where is my pelvic floor, where are those muscles and what are they doing?
Dr. Meagan:
Yeah. Yeah. I tend to also see a lot in the clinic where women have become what we call paradoxical or exactly the opposite because in their brains they want to lift up when they’re inhaling, because they want in in in all to go together, and in doing so they actually manipulate both the diaphragm and the pelvic floor to be coordinated exactly opposite of what we want and it’s this constant then tug of war and the pelvic floor just kind of freaks out and quits either by shutting off and allowing leaks or by spasming and tightening up to try to prevent them. That dysfunction kind of shows up.
Coach Stasi:
Oh, interesting. Yeah, so kind of the extremes that we had for our overachievers out there that they have been doing too much or too hard for for years over time.
Gennev:
You can now manage your menopause with Gennev. We’ve helped thousands of women take control of their health with our team of doctors, coaches and products. Join our membership program called HealthFix and work with one of our menopause coaches on your personalized menopause plan. Learn more at Gennev.com.
Coach Stasi:
Well, and it sounds like there’s opportunities for both sides. There’s prevention. So if women are in perimenopause or even pre-menopause, which I’ll admit, I’m pre-menopause, I’m 36 years old, still menstruating regularly, but it’s, so much of this is important for preparing. So I’m thinking a lot about, I know probably in the next 10 years there’s going to be some changes. And so would you say that doing these types of exercises, being aware of the pelvic floor, even before menopause, or definitely in peri-menopause is beneficial for women’s health?
Dr. Meagan:
Definitely. You know, I think across the whole lifespan, you know, I think, I think this is one of those muscle groups that we just kind of take for granted. You know, until there’s a problem with it, it’s off our radar, you know, and I think there’s a little bit of attention postpartum and then it’s like, unless again, unless it’s causing a major problem, we, it just loses focus. But you know, it’s a muscle. It’s a muscle group, use it or lose it. Right?
So I think by having a, a mindful focused approach on including the pelvic floor in your regular exercise routine, you can definitely help counteract some of the loss of muscle health and function from that reduction in estrogen. So I usually try to get women to the point of you know, if you’re, if you’re following a good exercise program and doing a mix of, you know, strengthening and conditioning if you are breathing correctly, correctly and including your pelvic floor during the task that you’re doing, those count as your daily pelvic floor exercises. You know, not everyone necessarily has to sit and do three minutes of Kegels, driving Kegles, uou know, all of the things that often time, you know, we are led to believe is necessary.
But if you can weave it into your day, all the better. And then you’re also gaining the functional benefit of, of your body learning and knowing how to use your pelvic floor to give you stability when you pick up your grandchild or push the door open or all of those things.
Coach Stasi:
That’s great. That’s great to know. It’s great to know that it doesn’t have to be a separate thing. Cause a lot of the women I work with, it’s, they’re already dealing with a lot. And so adding one more thing, like now you have to do Kegel exercises, even if it is just three minutes can really be another straw that breaks the camel’s back. So that’s helpful to know that recommending just breathing appropriately, which has, benefits in so many other areas too, can help them to target that and just bringing mindfulness and focus to that.
Dr. Meagan:
Yeah, no, don’t get me wrong. You know, if you’re in pelvic PT, you’ll be, you’ll be spending some time doing those specific exercises. But like I said, I like to get gals to that point where it’s just integrated in your day because then it actually happens, then it’s not something you have to remember to do.
Coach Stasi:
Yeah, exactly. Well, let’s talk about that. That’s a great point as well. And this is helpful for me, but if someone is that our listeners are listening to this, maybe thinking, Hmm, should I see a physical therapist for this or should, can I just focus on breathing and be, okay? Where’s the line where it’s like, you know what, having someone that’s watching you, giving you instruction where you have an appointment that you’re going to and potentially could provide additional therapy where, where’s the line? Or how did, how do women decide that?
Dr. Meagan:
So that’s a little tricky, right? I’m a pelvic PT, so I think everyone should come see a pelvic PT. I think that, you know, knowing that so many women are, or doing something just so subtly wrong that can really make or break their success that, you know, even just a single consultation with a pelvic PT can be so tremendously valuable to make sure that you aren’t making matters worse.
You know, I, I see women every single day where there, you know, maybe doing a sneaky breath hold in their Kegel and then they wonder why they are still leaking, when they even tried to do a Kegel you know, as they sneeze, it’s like, well you’re actually holding your breath, which is pushing down and your pelvic floor can’t combat the forces there. So so I think having another set of eyes to give that feedback is, is just, you know, priceless.
You know, public PTs are gaining accessibility. For a long time, you know, we were kind of far and few between, but I do feel like you know, there are some, some good resources out there for people to find pelvic PTs. You know, like our national organization, the American Physical Therapy Association has a website. Like find a PT: you can put in “women’s health and pelvic PT,” put in your zip code or city and it can help you locate someone who has good training and resources as close as possible.
Coach Stasi:
Oh excellent. Thank you for that resource. Cause I think that’s helpful with us working with women all over the country. How they know, okay, you know, if I’m looking for a physical therapist that specializes in this, how do I find them? And that’s also a great point: Knowing to ask it, it sounds like they shouldn’t just go to any PT clinic and say I need physical therapy. They should be saying, I want to work with a physical therapist that has expertise in pelvic health. Is that correct?
Dr. Meagan:
Yes. Yeah. Yeah. you know, we do get exposure in our professional training, but like I mentioned, the vast majority is in kind of that postgraduate, continuing education work.
Coach Stasi:
And can you talk a little bit about that? What makes, what have you done to become an expert in this area? What that additional training looks like? So, you know, it helps our listeners to understand and also to make sure that they aren’t going to someone that perhaps doesn’t have that expertise and potentially do more harm.
Dr. Meagan:
Yeah. So there are, there are various groups that offer continuing education. Most of them provide two to three day courses on the weekend where PTs will attend. And it is learning both the kind of didactic information and in depth learning of anatomy, physiology, what’s normal, what’s abnormal, what’s common and what’s uncommon. That combined with extensive lab practice where these physical therapists are practicing on each other. You know, so we’re learning as a patient, someone is doing these exams or these techniques on another PT so that you, you have that experience and that kind of level of understanding to know what, what the person on the table is also going through as you’re providing the services. You know, and, and typically it is then a sequence of courses that most people will end up going through depending upon their interests. You know, if they have more interest in bowel function or dysfunction, pregnancy, postpartum care, pelvic health but, and even in the introductory classes the therapists are going to be exposed to treating urinary incontinence, bowel incontinence, pelvic pain, painful intercourse. All of the things that we, we tend to see women in the clinic for.
Coach Stasi:
Okay. Yeah. So, and, and it sounds like there might be specific approaches for each of those things. So it’s not just a blanket approach for pelvic health. It’s what is your specific concern and here’s the approach for you.
Dr. Meagan
Definitely. Definitely. Yeah. Yeah, yeah. I was going to circle back to what you were saying about knowing if you need a pelvic PT within the last question. And as I was listing those things off, I think that’s, that’s kind of a nice, nice, way to put it on the radar is if you’re leaking anything, out of your vagina or your anus, involuntarily, that’s not normal. And that’s not okay. You know, it may be common and it may be brushed off because of, you know, whatever reason your mom or grandma may have told you. But absolutely there are things that can be done about it that are conservative and quite effective. If you’re having any pain, painful gynecological exams, painful wiping you know, with bowel movements or after urinating, any kind of painful vaginal penetration for intercourse. That should not hurt. And those are also indications that finding a PT you know, as well as working with your, your medical, other medical providers, but definitely things that, that pelvic PTs treat, I think are good to have, good to have on the radar and seek, seek more help.
Coach Stasi:
Yeah, absolutely. And I appreciate you listening out those symptoms because you make a good point. A lot of times, and I see this in a lot our, our Facebook group and when women are talking with each other, they have great community support, but sometimes when everyone in the community is experiencing pain and incontinence, they normalize it. And while it may be, I don’t, I don’t want to say no, I hesitate to use the term normal, maybe common, like you said, during this time of life. And, but it does attention and it doesn’t have to be the normal. It shouldn’t and it isn’t normal. And really does deserve treatment and there’s treatments out there and there’s no shame in it. You know, I think that’s the other part. Sometimes women when I’m talking with them may feel a little hesitant to talk about things that are going on in that area. But it’s important to know that’s a really important part of health and not to feel shame and to know that they can get support.
Dr. Meagan:
Most definitely. Yeah. Yeah. Most of the women that I end up seeing and talking to in the clinic tell me, Oh my gosh, I wish I would’ve known this five, 10, 20 years ago. You know, it’s, it’s again, I think it’s gaining you know, its ability to be talked about more comfortably and knowledge is power. But yeah, you’re right. It still is something that for some reason women are felt to, to feel, you know, some, some personal level of shame about, but should not.
Coach Stasi:
No. And that’s where we’re hoping here at Gennev to kind of change that perception of menopause, this time of life, and really provide the resources that are out there. And based on what you said, it sounds like most women, if not all, should have a pelvic floor PT on their healthcare team or on their menopause support team during this time in their life. I mean, it’s putting the tool in the toolbox to really help them thrive.
Dr. Meagan:
Yes, most definitely.
Coach Stasi:
Excellent. Well, I really appreciate your time today. Is there anything else that you want to add or last tips or points? And give your clinic information and location for any listeners that may be near you just to finish up with.
Dr. Meagan:
Yeah, I mean, I think you know, thank you for having me. I think it’s just awesome that we’re getting the word out and, you know, like I said, knowledge is power and, and knowing that there’s hope and that it doesn’t mean that you have jump on a medication. It doesn’t mean you have to jump to surgery. You know, and there there’s always the potential to make these even slight improvements and, and it’s not, it’s not terribly hard work to do once, once you get committed to it. It’s just a lot of, a lot of changing and bringing things to awareness that can have pretty profound positive impacts on people’s lives.
I practice out of Orthopedic and Spine Therapy. We are a private practice in Wisconsin in the Appleton, Wisconsin area and we have clinics kind of scattered throughout the state but pretty much focused in the Fox Valley area.
Coach Stasi:
Okay, excellent. Well good information for our listeners to locate you or certainly you gave them the information and that was the what was the, the organization is the, the American Physical Therapy Association?
Dr. Meagan:
Yup. APTA.
Here’s to better pelvic health and wellness
Coach Stasi:
Okay, excellent. And you can go on there, put in your zip code and then specifically look up women’s health and pelvic health to find someone that is trained in that.
All right, well just to finish up on my end, I do want to put a plug out there for our HealthFix program. I am a menopause coach as I mentioned in the beginning working with that program. And having that membership, it’s a subscription based membership, you get the opportunity to work with someone like myself and talk with them out through calls as well as have supported accountability between those calls. And so it can be an opportunity as well if you’re thinking, I don’t know if I should go see a pelvic PT even though I think after this we all should, but if you have questions about that or just questions about any symptoms you’re experiencing during menopause, signing up for the HealthFix program gives you the opportunity to have some of those questions answered, provide resources, information and support around finding what the next steps are. Perhaps it’s finding that physical therapist in your area or perhaps it’s just figuring out what that next step is for you, whether it be pelvic health or other menopause symptoms. So sign up for that HealthFix program and I hope to be working with more of you that are listening to this podcast today. So thanks very much Meagan, and I hope you have a great rest of your day and I’m sure we’ll collaborate again soon.
Dr. Meagan:
Wonderful. I look forward to it.
Coach Stasi:
All right, take care.
Dr. Meagan:
Thank you.
Gennev:
Thank you. Thank you for listening to this episode of the Gennev podcast. Remember, you can subscribe on iTunes, Google play, Spotify, and just about anywhere you get your podcasts. Gennev is your online destination for menopause, doctors, coaches, products, and education. You can find us at Gennev.com. Thanks for joining.
Learn more from Coach Stasi Kasianchuk and Dr. Meagan Peeters-Gebler by searching on their names on this site.
If you have issues with your pelvic floor or have improved your pelvic health, we’d love for you to talk with us about it. Please join us on the Gennev Community forums!
