When we talk to women about what would have the greatest beneficial impact on their quality of life, there’s one answer that seems to stretch across the entire menopause experience:
Sleep.
It affects everything about our lives “ our mood, our energy levels, our productivity, our confidence, our weight, our physical and mental health in menopause “ for good or ill.
Not enough quality sleep can lead to serious medical conditions like high blood pressure, heart disease, and diabetes. Our immunity can be challenged when our sleep tanks, and that’s especially bad right now.
The occasional sleepless night is uncomfortable but not particularly harmful (unless you doze off while driving “ please don’t do that), but many women we talk to feel like they haven’t had a decent sleep in years. And that takes a real toll on body, mind, and joy.
There are lots of reasons women sleep poorly in this time: hot flashes/night sweats, anxiety, restless leg syndrome, urinary issues, pain”¦. Women in perimenopause and post-menopause have difficulty falling asleep and staying asleep, and they wake up more tired than they were the night before.
Unfortunately, sleep disruption doesn’t usually disappear along with other menopause symptoms. Poor sleep can also be a result of simply getting older. But good news: we can help.
How To Get Better Sleep During Menopause
For many women, a truly effective solution is cannabidiol or CBD. One of many components of the hemp plant, CBD is being studied for a wide range of health benefits, including managing some seizure disorders in children, but also potentially heart disease, some cancers, even dementia.
And while the scientific community is still researching CBD to determine its efficacy, so many women asked us to create a safe, smart supplement, that we jumped into the research with both feet.
Here’s what we learned:
Reported benefits
For many, CBD can help reduce pain, depression, and anxiety and promote relaxation.
How? Well, our bodies already produce endocannabinoids, nuerotransmitters that bind to cannabinoid receptors present in our nervous systems. It’s possible that CBD reduces pain by interacting in that process and reducing inflammation.
And here’s a hint: add a magnesium glycinate capsule to your pre-bed routine for even more natural pain-relief, sleep-promoting assistance.
When it comes to anxiety and depression, CBD may be acting on the brain’s serotonin receptors, imitating the “feel-good” properties of the neurotransmitter. By alleviating pain and worry and promoting relaxation, CBD may be making it a whole lot easier to fall asleep.
Adding melatonin
Our bodies naturally produce the hormone melatonin in the evenings as sunlight diminishes. It helps our bodies and minds relax and prepare for sleep.
However, melatonin production declines with age, making good sleep harder to come by. Adding back some of the lost melatonin may help you fall asleep sooner, stay asleep longer, and get better quality sleep, says the Mayo Clinic
Melatonin may be of particular help if you travel a lot and have to deal with jet lag and time zones, or if your work shift hours dictate sleeping in the day and working through the night.
According to Gennev Naturopathic Physician Dr. Wendy Ellis, 1 mg is typically the amount that provides restorative sleep without the next-day “hangover.”
“You want to mimic normal physiologic doses (the amount the body makes on its own) as much as you can, and most studies say that is 0.3 to 0.8 mg per day. Three milligrams or 5mg is typically too much,” she says.
Legality, side effects, concerns
If you’re concerned about taking CBD, the following information might help.
Cannabidiol (CBD) as which comes from the hemp plant, not from the marijuana plant “ does not have psychoactive properties and is legal in all 50 states in the US. It is considered generally safe. In fact, the World Health Organization says, “In humans, CBD exhibits no effects indicative of any abuse or dependence potential”¦. To date, there is no evidence of public health related problems associated with the use of pure CBD.”
Side effects can include nausea, fatigue, and irritability, says Harvard Health; if you’ve been warned away from grapefruit because of its blood thinning effect, you should avoid CBD products as well.
The greatest concern around CBD for most medical professionals is that it’s unregulated, so it can be difficult to know exactly what you’re getting. Be sure you’re getting CBD from a reliable source.
And of course, we always recommend letting your doctor know you’re adding something new “ just in case there are any concerns the CBD and/or melatonin may interact with medicines you’re taking or health concerns you have.
One of the problems Gennev is out to solve is the lack of information many women run up against when they try to research some strange new thing their body is doing. (Cold flashes in menopause? Who knew those even existed?!)
One concern we hear about from women is bleeding months or even years after a woman is in full menopause. Bleeding after menopause, like many things in midlife bodies, is probably not caused by anything dangerous. However, any bleeding after menopause isn’t normal and can signal something more serious.
We talked to Dr. Jessie Marrs of the Swedish Cancer Institute. Board-certified in obstetrics and gynecology with a special interest in women in menopause, Dr. Jessie was able to give us some very comprehensive answers to some very important questions.
What is post-menopausal bleeding?
Dr. Jessie: First, let’s start with a definition so we all know we are on the same page. When someone goes through menopause, it essentially means their menses have stopped.
Women are considered “menopausal” when they have had no period for an entire year. This definition is important because it also helps us define post-menopausal bleeding which can have some important implications.
Why does post-menopausal bleeding happen?
Dr. Jessie: Post-menopausal bleeding (PMB) can happen for a variety of reasons. Sometimes it is from tearing of the vaginal tissues after intercourse. It can happen because of polyps or fibroids in the cervix or uterus.
Some women will develop such a thin lining of the uterus after menopause that they can bleed a little bit. Medications, such as hormone replacement therapy, anticoagulants or tamoxifen can also cause bleeding after menopause.
Occasionally it is related to pre-cancer or cancer of the lining of the uterus. This is obviously the thing we worry most about. The good news is, cancer of the uterine lining (endometrial cancer) generally presents early with vaginal bleeding and is often curable. This is why it is important to see your doctor if you have any bleeding after menopause.
If you are bleeding after menopause, a Gennev menopause-certified gynecologist can give you a trusted opinion, determine if medication is right for you, and they can provide prescription support. Book an appointment with a doctor here.
What is the most common cause of bleeding after menopause?
Dr. Jessie: About 40 percent of bleeding after menopause is caused by non-cancerous polyps in the lining of the uterus. The second most common cause is vaginal atrophy or thinning of the uterine lining.
How can I distinguish more serious issues from spotting after menopause for other reasons (post-coital tearing, etc.)? Are there other warning signs?
Dr. Jessie: It can be very challenging to distinguish pre-cancer or cancer of the uterus from other causes without an exam. Things like weight loss, pain or persistent bleeding are more likely with advanced cancers.
Bleeding without any other symptoms can be a sign of early cancer. Because of this, I don’t recommend trying to decide for yourself where your bleeding is coming from. It is always worth seeing your doctor for this issue.
Can fibroids cause bleeding after menopause?
Dr. Jessie: Yes, although this is unusual. Most fibroids shrink after menopause and become less symptomatic than they were prior to menopause.
Fibroids that are pushing in to the cavity of the uterus can certainly cause post-menopausal bleeding, but I usually see this in patients who are in their early 50s; they think they are not menopausal because they continue to bleed, but the bleeding is actually coming from the fibroid and not a hormonal cycle.
I don’t usually see bleeding from fibroids starting up when a woman is already well in to menopause. If you know you have fibroids and are having bleeding after menopause, I would definitely recommend a visit to your doctor rather than writing the symptoms off as coming from the fibroids. Very rarely, women can develop a fibroid-related uterine cancer called a sarcoma.
Is any post-menopausal discharge normal?
Dr. Jessie: Most women develop some level of vaginal dryness after menopause. This is related to the decreasing hormonal effect of estrogen can create vaginal issues and changes and effect tissues. Some discharge can still be normal, particularly if it is white, clear or creamy in texture. Copious amounts of watery discharge, bloody, or even brown- or pink-tinged discharge would be considered abnormal.
Does it matter how far after menopause you are? Say, six months post-meno as opposed to six years?
Dr. Jessie: It doesn’t. Post-menopausal bleeding can be an indicator for abnormal cells in the uterine lining at any point after menopause. While there are probably more benign conditions that can cause some vaginal bleeding the closer you are to menopause (including a late burst of hormone from the ovaries), if you have gone a full year without a period, you need to get in to see your doctor.
I have spotting after menopause on my underwear; what do I do?
Dr. Jessie: Please call your doctor and make an appointment. As long as the bleeding is minimal, this is not an emergency, but I like to get patients in for this problem within the next week. While seeing your gynecologist is generally not as fun as, say, buying some new shoes (yes, that is my weakness), the work up for post-menopausal bleeding is pretty straight forward and can bring some peace of mind.
Does it matter if it’s heavy or light? Is just a little spotting OK?
Dr. Jessie: Great question, I frequently have patients delay seeing me for bleeding after menopause because it was a small amount. Even the smallest amount of vaginal bleeding after menopause is considered abnormal and deserves a work up.
What will the doctor do if I tell her I have post-menopausal bleeding?
Dr. Jessie: When you come in to the office for bleeding after menopause, your doctor will take a thorough history to get a better idea where the bleeding might be coming from. She will do a physical exam and inspect the vulva, vagina and cervix to look for a potential source of the bleeding. She’ll also do a pelvic exam to see if the uterus feels enlarged or the ovaries feel abnormal.
Because PMB is a warning sign for pre-cancer or cancer of the lining of the uterus, even if she finds a likely cause during the exam, your doctor will do some sort of an evaluation of the lining of the uterus. This may be an ultrasound to determine the thickness of the lining or it may be a biopsy of the lining of the uterus.
Can I wait and see if it happens again before going to my doc?
Dr. Jessie: Please don’t wait! It is very likely that your bleeding is nothing to worry about and just a nuisance, but occasionally it can be a sign of something more serious. It is always worth a check-up!
If you’re experiencing post-menopausal bleeding, please follow Dr. Jessie’s advice and schedule an appointment right away. If you don’t have an ob/gyn, you book a virtual appointment at Gennev Telehealth. If you’ve dealt with PMB, what caused it and how did you deal with it? Please share with the community: leave us a comment below, or talk to us on our Facebook page or in Midlife & Menopause Solutions, our closed Facebook group.
This transition in your life can be very drying as menopause can cause dry eyes, hair, a dehydrated mouth, itchy skin, dry vagina. As estrogen diminishes, so does the amount of moisture available and our body’s ability to suck it up and retain it.
In none of these places is the dryness really welcome: dry eyes can fog our vision; dry skin itches and wrinkles, and a dry vagina can make penetrative sex unpleasant, even painful.
If you are thinking about a vaginal dilator for painful sex, consult with a specialist. A Gennev menopause-certified gynecologist can give you a trusted opinion, determine if medication is right for you, and they can provide prescription support. Book an appointment with a doctor here.
Menopause Painful Intercourse
The vagina doesn’t just get drier in menopause; it can actually get narrower, shorter, and less flexible. All of these can contribute to pain during sex. And, as we already know, there is no shortage of causes for hurtful sex, especially painful sex after pregnancy or throughout menopause and perimenopause (even intercourse after menopause).
Fortunately, vaginal dilators are a good tool for managing these changes. To get the best results, you’ll need the right equipment, a little training, and some patience. With time, you may be able to increase the width and depth you’re able to tolerate (even enjoy!) and restore some elasticity.
We strongly recommend you start by consulting a pelvic physical therapist, if possible. A pelvic PT can tell you if something else is causing your pain (like pelvic organ prolapse) and advise you on how to proceed with dilators.
A couple of things to make clear: feeling ashamed or as if you’ve somehow failed is neither necessary nor accurate. These changes in the body are normal, though women and their partners don’t have to live with them. Many women don’t get help for vaginal dryness or atrophy because of embarrassment “ they’re even too ashamed to talk with their own doctors.
Women around the world are raving about Gennev’s Intimate Moisture. We designed a lubricant for sex so you can start enjoy yourself again.
You can go down the vaginal dilator path completely on your own, as they don’t require a prescription. But we recommend you talk about it with your ob/gyn or one of ours to eliminate other possible causes and get instructions on how to proceed.
What are vaginal dilators?
Dilators are generally made of plastic, rubber, silicone, or glass, are tube shaped, and come in a set of 5 to 8 graduated sizes. Inserted in the vagina, they gently stretch the vaginal walls over time.
Dilators range in size from half an inch in circumference for the smallest to just over an inch and a half at the largest. They are smooth-surfaced, rounded at one end, and may come with an interchangeable handle for easier use.
Who are dilators good for?
Most women use dilators to enable them to enjoy vaginal sex again, though they may also be used to prevent or reverse atrophy due to lichen sclerosis flare ups or menopause. Women who have a fear of pain due to cystitis or other factors may also find dilators help them relax, as it puts them in control of the level, pace, and timing of penetration.
Additionally, women who have had cancer may find changes in the vagina beginning as a result of treatments or surgery; starting with dilators as soon as possible may help avoid vaginal atrophy from developing or worsening.
How To Use Vaginal Dilators For Atrophy
You want to ensure maximum relaxation, so be sure you have plenty of time and privacy. Using vaginal dilators for atrophy generally takes between 10 and 15 minutes.
Our ob/gyn Director of Health, Dr. Rebecca Dunsmoor-Su, says women in perimenopause and menopause should always always use a lubricant when inserting anything into the vagina. As long as your dilator isn’t made of silicone, a silicone-based lubricant is best, as silicone stays slippery longer. If your dilator is made of silicone, stick to water-based lubes like our Personal Lubricant to avoid damaging the dilator’s surface.
Unless a pelvic PT tells you otherwise, it’s usually best to start with the smallest dilator in your set. Lube it up, then lie on your back with your knees bent, feet flat, and insert the dilator as you would a tampon. But go slowly, applying gentle pressure. If you feel any pain, stop. You should feel pressure only as never pain. If you don’t feel much of anything, you may need to try the next size up.
The Memorial Sloan Kettering Cancer Center suggests doing Kegels to help you insert the dilator, as these exercises can help relax your pelvic floor muscles. You can also do Kegels during the process, as it may allow you to go in a little farther.
Once inserted, you can push in and pull back on the dilator to gently stretch the length of your vagina. Soft circles can help with increasing width. Feel free to add more lubricant as needed to keep things comfortably moist. About 10 minutes is all you need at one time. Sloan Kettering advises using moisturizers in the intimate area every night before bedtime to keep things pliable.
Once you’ve finished, remove the dilator, wash with warm, soapy water, and store according to your dilator’s instructions.
Advice differs on how often to use the dilators, but at least 4 times a week seems like a good average. If there’s no pain or irritation, you can probably do more, though too many days in a row isn’t advised. Be patient. Use each size for several weeks until the next size up causes no discomfort. It may take several months to achieve the results you want.
You may have some bleeding after using dilators; this is normal. An amount of blood easily handled by a panty liner is normal. Enough blood to soak a pad or bleeding that lasts longer than one day are flags. Please talk with a doctor immediately if you notice excessive blood or bleeding that lasts too long.
How do you choose them?
Like so many things, there are a dizzying array of options. We suggest you find a good site that offers not just products, but good information and advice. Dr. Rebecca really likes Seattle-based Babeland for its very no-nonsense, informed approach to healthy sexuality.
Dr. Rebecca also suggests sets that come with a vibrating wand that cam help with relaxation, even add pleasure. Babeland offers the Intimate Basics Dilator set, which is on Dr. Rebecca’s list of good options.
If you’ve used a dilator, we’d love to hear how it worked for you. Feel free to tell us about it in the comments below, find us on Facebook or in Midlife & Menopause Solutions, our Facebook group.
At Gennev HQ, we joke that Burning Mouth or burnt tongue syndrome makes us think of Burning Man.
It’s not funny though: if you’ve ever gulped too-hot coffee or bitten into a pizza fresh out of the oven, you know the serious pain of a burnt tongue.
And for some of us, this sensation happens without any known cause or injury.
If you feel like you’ve scalded your mouth and just can’t remember when or where, it may not be midlife brain fog: there really might be something going on, even if you (or your doctor) can’t pinpoint the source.
It’s called Burning Mouth Syndrome (BMS) and, for some reason, people in perimenopause are more likely to experience this symptom
What is Burning Mouth Syndrome?
BMS is, in medical terms, a “chronic orofacial pain disorder.”
BMS symptoms include feelings of burning (hot, tingling, and painful), other paresthesia or tingling all over the body (abnormal sensations of the skin, like prickling, tickling, chills, or numbness), and pain inside the mouth without an obvious lesion or injury.
Most sufferers feel pain on the front part of the tongue, but the roof of the mouth, palate, gums, lips, and other tissues may also be affected.
People with BMS may also experience dry mouth, sensitivity to certain foods, and strange tastes.
While some infections, medications, diseases, nutritional deficiencies, dental work, or psychological conditions are known to cause these symptoms (called secondary BMS), primary BMS is idiopathic: there isn’t a discernible cause. A third type may stem from an allergy to certain preservatives.
For sufferers with primary BMS, pain typically gets worse over the course of a day; people may feel fine when they wake up, and the discomfort peaks in the evening. With secondary BMS, the pain remains consistent.
We don’t know why primary BMS happens, but research suggests that it’s possibly due to nerve fibers malfunctioning, potentially those in the back of the head or in the front of the tongue.
Overall, Europeans are more likely to experience BMS than Asian or American residents (7% prevalence vs. 2-3% and 0.7%, respectively).
Anyone can get BMS, but because a disproportionate percentage of sufferers are perimenopausal women of all races and backgrounds, experts suspect that hormonal changes are be involved. Depending on who you ask, anywhere from 10% to 40% of menopausal women may experience BMS, though different diagnostic criteria are not well-defined.
This hormonal tie-in does make sense: like your genitals, the mucous membranes in your mouth have sex hormone receptors, and we know that decreases in estrogen around menopause and dry mouth can lead to both decreased saliva production and the periodontal issues associated with dry mouth.
Other potential causes or links to BMS include oral parafunctions (like clenching your jaw or grinding your teeth), an allergy to dental materials, diabetes, vitamin B, folic acid, or iron deficiencies, gastrointestinal diseases, psychiatric and neurological disorders, or pharmaceutical side effects.
In up to a third of cases, multiple causes are suspected.
While BMS caused by hormonal changes isn’t dangerous, it can lead to people not eating or not eating well. Alternatively, for those who find that eating or drinking temporarily reduces the pain of BMS, the condition can lead to overdoing it and consuming more than is healthy.
Great. So what can I do about my BMS?
Like many benign conditions, BMS won’t kill you, but it can make your life miserable. The discomfort can disrupt your sleep, make it difficult to eat, and lead to anxiety and menopause depression.
The bad news is that treating BMS is mostly managing symptoms. The good news is that you have options.
See your doctor and your dentist! They’ll want to rule out all other potential causes, like some anti-depressants (dry mouth), Alzheimer’s, Parkinsons, or hypothyroidism (change in taste), lichen planus (sores) or a yeast infection (redness). Experts recommend examination of teeth, mouth, temporomandibular joint, and dentures (if applicable), as well as a full blood count, tests for folic acid, iron, B vitamins, sex hormones, and blood sugar and swabs for oral bacteria.
Fight fire with fire. Believe it or not, spicy foods can actually help BMS: capsaicin (the compound that makes hot peppers hot) can disable the pain-signaling chemicals in nerve cells. You can buy capsaicin oil over the counter or you can put a few drops of Tabasco sauce in a teaspoon of water and swish this around in your mouth. Too good to be true? Menopause Goddess Lynette Sheppard swears by capsaicin.
Quit smoking. When we said “fight fire with fire,” smoking is NOT what we had in mind. BMD can be triggered by tobacco, so cutting down on cigarettes, cigars, and even chewing tobacco could help reduce the incidence and/or severity of BMD symptoms.
Avoid carbonation. A cool drink may sound terrific, and maybe it will help, but choose non-carbonated liquids or plain ice water, as carbonation does worsen BMS in some people.
Manage stress. The relationship between stress and BMS and other chronic disorders is a little bit of a chicken-and-egg situation. Does your BMS cause stress, or does stress in menopause cause BMS? Regardless, stress is bad for your health. Yoga, meditation, exercise, psychotherapy, and cognitive-behavioral therapy have been shown to lessen BMS discomfort.
Try alpha-lipoic acid (ALA). Your body naturally produces this antioxidant, and it’s also found in foods like tomatoes, potatoes, and spinach. ALA promotes the production of nerve growth factor and is typically used to treat diabetic neuropathy and other nerve issues “ potentially including BMS. While studies suggest improvement in BMS symptoms compared to placebo, more research is still needed.
Hormone replacement therapy. We’ve written many times before about our stance on hormone replacement therapy HRT has many pros and cons.. If this is something that works for you and your doctor, hormone replacement therapy can help BMS.
Struggling with BMS? A Gennev menopause-certified gynecologist can give you a trusted opinion, if medication is right for you, and they can provide prescription support. Book an appointment with a doctor here.
BMS is no picnic, but you have support and choices in how you manage it. Talk with one of our menopause-specialist doctors about your options for controlling your menopause symptoms via Gennev’s telemedicine service.
Do you suspect you may have primary or secondary BMS? We’d love to hear about your experience in our Gennev Community forums.
While on a birthday trip to Bermuda, Rolonda Wright wasn’t feeling well. VERY not well. Constipation turned to abdominal pain bad enough to send her to the ER for 15 hours.

On her return “ after a vacation that wasn’t at all what she’d hoped for “ she went to her great OB/GYN for tests and discovered she had a uterine fibroid “the size of a four-and-a-half-month pregnancy” or, as Gennev CMO Dr. Rebecca Dunsmoor-Su translated: about a personal-sized watermelon.
Sitting up high, it was actually visible as a bump when Wright was lying down.
“That’s not at all uncommon,” says Dr. Dunsmoor-Su. “So many women come to me with large fibroids thinking they’ve been eating too much bread. It’s not bread! It’s a big ball of muscle.”
“I thought I had to do more sit ups to get that ab down! A doctor a few years ago suggested a hysterectomy for my fibroids, but I didn’t really have any problems: no pain, no problems with sex,” Wright says. She had heavy periods, but the heavy flow only lasted for a day. “One day I couldn’t leave the house or it would have been a disaster, but the next day it was fine.”
The problem, she says, wasn’t so much the fibroid. It was how little information she had. She came to Gennev to share her journey with us and our readers so that other women would be better informed. You can follow her journey on Facebook, Instagram, TikTok at Rogirll01, or her website.
When you know more, you can act faster, she says. She might have had the fibroid removed when it was much smaller and required less invasive surgery. She might have had a hysterectomy years ago and had a much better time in Bermuda.
Dr. Rebecca Dunsmoor-Su Answers Hysterectomy Questions
Hysterectomy is a big deal, and no one should make the decision to have one without all the information they need and want. So before Wright went in for hers, she came to ask to the questions that should have been answered long ago.
What follows is a very important conversation between Rolonda Wright and OB/GYN and menopause specialist Dr. Rebecca Dunsmoor-Su. Rolonda Wright’s questions are in italics.
How do I prepare for this, both mentally and physically? This housed my child, so it is a little bittersweet. I’m good with it, I’m ready for it, but it’s also a subtle loss.
“It’s a transition,” says Dr. Dunsmoor-Su. “This marks a new stage in your life, and while that’s a good thing, it’s also a loss. You can be happy and sad at the same time.
“I’m glad you’re doing this and sharing this because women put up with a lot: we endure the pain, the bleeding, the discomfort for such a long time. Partly this may be because it increases slowly and gradually over time. If we went from a normal period to a super heavy period in one month, we’d see a doctor. But because it happens incrementally, we feel like it’s a normal part of aging. So I’m glad you’re bringing this to women’s attention.”
That’s part of the reason I came to you. I’m not even sure what questions I should be asking right now. What do I need to know?
“First, there are multiple kinds of hysterectomy. As physicians, we tend to define it by route of hysterectomy: both by how are we going to do the procedure, and also by what we’re taking and what we’re leaving behind, like ovaries or cervix.
“Fibroids are balls of uterine muscle that grow in the wall of the uterus. They can grow very large. And they are progressive, as they’re estrogen-stimulated. So as long as there’s estrogen in the system, they will continue to grow. We tend to see particularly quick growth through perimenopause when women get these really high spikes of estrogen. So a lot of women end up sort of in that perimenopausal stage, coming in to see us because suddenly this thing has grown quickly.”
Why do Black women have more fibroids than white women?
“Unfortunately, this is one of those things we don’t understand. Black and Asian women tend to have more fibroids; there are thoughts about vitamin D lack and other things, but the research just isn’t sufficient to draw conclusions.
“Not only do Black women have more fibroids, they’re more frequently undiagnosed or misdiagnosed and improperly treated because of systemic racism and sexism in medicine. And because Black women are used to being treated poorly by medical professionals, they may not seek treatment as early. Which is so unfortunate, because the sooner fibroids are caught, the more easily they can be treated.”
I’m a few days prior to surgery. What do I need to be thinking about now?
“In the days prior, you should know how your surgeon is going to do the surgery. It matters because different surgeries have different recovery periods. So if you don’t know, be sure to ask. Also, how are you going to recover? How active can you be, and how quickly? Who’s going to help you out at home, especially in the first couple of days?
“This is even more important now, in the time of COVID, because you need to take extra precautions. Anyone you come in contact with needs to be wearing a mask and washing their hands frequently, and so do you. If they can be tested for COVID and minimize contact with others, that’s best.”
So why have a complete hysterectomy?
“We do hysterectomies because the surgery is much simpler, and generally the women we see are done having children. It’s possible to preserve the uterus for women who are still planning to bear children, but it is a much more complicated, much more difficult, and much higher blood-loss surgery than just removing the whole uterus. Also, you never have just one fibroid. We usually can see one, but there’s always other fibroids in the wall.
“Additionally, fibroids will continue to grow. So we could do the surgery, take the fibroids out, and in two years you could be right back where you are now. If there’s a need to keep the uterus, then we would do the myomectomy, which is the removal fibroid surgery. But if you’re done having children, the hysterectomy is quicker, safer, and has an easier recovery.”
Should I keep my ovaries and fallopian tubes?
“In most women who are having surgery for fibroids, we don’t remove the ovaries, because there’s no reason to put someone into sudden menopause when really the only problem is the fibroids. We usually take the tubes now because there’s some question about whether they contribute to ovarian cancer rates. However, we usually leave at least one or both ovaries because then you drift into a gradual menopause. Your ovaries also have some roles after menopause in terms of making precursor hormones and testosterone. Those are good, so we want to preserve that function if we can.”
Why do some women elect to have their ovaries removed?
“It’s always a balance of risk/benefit ratio. When I counsel patients, I ask, “Do you have a high risk in your family of ovarian cancer or familial breast cancer?’ Familiar ovarian cancer history could mean you’re at higher risk for ovarian cancer, so we might want to consider removing the ovaries.
“Also, if you personally had breast cancer, removing the ovaries can mean reducing the stimulation of the breast tissue with estrogen which can help prevent recurrence.
“But in most women who are just having surgery for something like a fibroid or heavy bleeding, and whose ovaries are not at particularly high risk, there’s a greater benefit to leaving them. Ovarian cancer doesn’t happen very often, especially in women with few risk factors. Whereas cardiovascular disease and bone fractures and all those things that come with menopause do happen quite often. And so drifting into a more gentle menopause at a later age is just more beneficial for women.”
What are the different methods of hysterectomy, and how do surgeons and women decide which route to take?
“It really depends on the reason for the hysterectomy and what your provider has been trained to use. It’s amazing what we can do without opening your abdomen anymore. Now that we have all these techniques and tricks. Some can be done vaginally, which means we go in through the vagina, grab it, snip it loose and pull it out. In those cases, women don’t even have an incision. And that works when the uterus is small, with no large fibroids. But when you have a larger uterus with large fibroids, we use the laparoscopic camera or the robot, depending on training. We make a couple of centimeter-long holes in your abdomen, and we can get that larger uterus out that way. We disconnect the organ with all the fibroids still in it, put it all into a bag to keep it contained, use a device to turn it into one long strip, then pull it all out. The bag is a precaution because rarely the fibroid can contain cancerous cells that we don’t want spreading throughout the body.
“The beauty of this is that the pain of surgery is generally from the incisions. When incisions can be kept really small, or when you don’t have to make them at all, the pain is much less and the recovery is faster. There will likely be a dull aching in the low pelvis, but women won’t have to struggle to recover nearly as much as previous generations.”
How is the uterus anchored inside the body?
“Generally speaking, it is anchored where the uterus and the cervix meet. If you think of the uterus as a fist, the cervix would be the wrist that hangs out into the vagina. It’s anchored at the connections or the point where the uterus and cervix are joined by two ligaments that go back to your sacrum or tailbone. There are tubes that come off the top of the uterus and sit around the ovaries, but they’re not really connected to the ovaries. There is a little vascular connection between the ovary and the uterus, and that’s pretty simple to disconnect. And then it’s mostly blood vessels.
“At the bottom of the uterus, we take the cervix and close the top of the vagina. Taking the cervix removes cervical cancer concerns, and there’s really no reason to leave it behind. It doesn’t had to do with sexual pleasure, nor does it provide support for the vagina, as was once thought.”
Will I feel any different without a uterus?
“Because your fibroid is quite large, you may feel the lack of the fibroid, but that’s a good thing! You’ll probably feel a bit thinner and less heavy, you’ll have less constipation, possibly less urinary urgency without that big thing putting pressure on your bladder or making constrictions. In terms of sexual pleasure, there shouldn’t be any difference. The center of women’s sexual pleasure is the clitoris, and we don’t remove that “ it’s very important! If your ovaries are not removed, you won’t have a difference in hormones.”
What should I look out for? Are there concerns after the surgery?
“Of course, every surgery carries risks, so let’s talk about them. There are three main things that I counsel about in terms of risks of any surgery and specifically a hysterectomy risk.”
“Number one is bleeding. Because of the fibroid, you have a big uterus; it’s got big blood vessels to feed it. So we have to tie those off properly. We’re performing the surgery under visualization, so we can see that nothing’s bleeding, but it’s not impossible for a blood vessel to be in spasm and not bleeding and then open up later. So if you suddenly feel dizzy or lightheaded or have severe abdominal pain, those are signs of internal bleeding.
“Number two is infection. We give antibiotics before surgery, and it’s not a big infection risk, but obviously high fevers, chills, and severe abdominal pain can be a sign of infection.
“The last one’s a little more vague. It’s damage to structures around the uterus. There’s bowel all around the uterus, and the bladder in front. Ureters are tubes that carry urine from the kidneys to the bladder, and they go down the side of the uterus and up and over it to get to the bladder. Experienced surgeons will identify them and make sure they’re out of the way and check them at the end, but rarely an unrecognized injury can happen.
“The most common unrecognized injury is actually to the ureter, that tube between the kidney and the bladder. As we’re coming down the side of the uterus to seal off the blood vessels, we’re usually using cautery because it seals the edge of the blood vessel and then we can divide it.
“If the cautery is just a little bit too close to the ureter, even if it wasn’t cut, it could have some localized thermal damage and that can show up a week or two later. That usually ends up presenting as severe abdominal pain, sometimes flank pain. That’s something to look out for as well.
“Again, all of these complications are very rare, but they can happen even to the best surgeon. If there were complications during surgery, your surgeon will let you know about it and tell you what to be on the alert for, but by and large, this is a low-risk surgery.”
What will happen as a result of the surgery? Am I going to gain weight or lose my hair?
“I tell women who are near to the menopause that for about six weeks after a hysterectomy, you may have an upswing in hot flashes. A lot of that’s just inflammation and healing; after all, the ovaries took a little hit! But it usually settles out, and you should drift into a natural menopause like you were before the hysterectomy.
“The best way to minimize problems in recovery is to go in healthy and really well nourished. Make sure you’ve got all the nutrients you need for your body to undertake this big healing process. I am not personally a huge supplement taker. I tend to eat a very balanced diet and that’s generally enough, but before my own surgery, I took Gennev’s Vitality product, which is a daily supplement. I used it for the months surrounding my surgery. I knew that I would be barreling through all these nutrients as my body’s trying to heal, so I wanted to do everything I could to help my body do that. Vitality is a very focused supplement for women age 40 and above, and it has the things we need more of like vitamin B and vitamin D and so on.
“Before surgery, I talk to my patients about their health goals, their history, and their risks because all of those should inform their surgery.
“Even though you may not go into menopause because of your surgery, you’re eventually going to go into menopause. How do you want to handle that? What are your fears about this process of menopausal transition? And, you know, what’s most important to you to preserve?
“You know, some women say my biggest fear is weight gain, in which case I say, well, there are a couple of really important things you need to keep in mind: One, you lose muscle mass as you go into menopause. So adding more weight training to your regimen rather than more cardio can help you maintain weight. Two, you need fewer calories as you get older.
“Is fear based around sexual function? In that case, I tell them there are important things they need to do during menopause. One is make sure your relationship and your stressors are under control because probably the most key things in any woman’s libido are stress and relationship stress. Number two, make sure vaginal tissues and happy and healthy and take pleasure from intercourse. We can do that by treating vaginal tissues with local estrogen or other moisturizers and using a really good lubricant. Do it right away, because once you start to experience pain down there, you may start to fear sex and it will drive your libido down.
“For some women, fear centers more around longevity in terms of cardiovascular health and bone health. Maybe they have a strong family history of osteoporosis or heart attacks. Then we talk about hormone replacement. Certainly if someone’s having significant symptoms around menopause, like significant hot flashes, significant sleep disturbances, HRT can really help them transition comfortably and safely.
“For many or most women, we experience menopause in our fifties, when we’re not done at work. We are at the height of our careers. We can’t really afford to be having seven hot flashes a day and not sleeping at night. So we take hormone replacement through our fifties and into our sixties and come off it when we retire. I have patients who use hormone replacement for two years. I have patients who use hormone replacement for 10 years. I have patients who use hormone replacement until they die because they love it and it makes them feel good. And all of those are appropriate responses to menopause.”
Rolonda Wright is sharing her journey with us so other women will have an easier “ and certainly more informed “ journey of their own. While we’re comfortable talking about all kinds of personal things (ask any runner about their digestive system, for example), hysterectomies have long been considered embarrassing and shameful. And that does not help women be healthier.
Our thanks to Rolonda for sharing her experience, asking questions so many women share but are too afraid to ask or have no one to ask. If any of her experience sounds familiar to you, we encourage you to talk to your doctor or ours to learn more. Don’t wait, don’t suffer, don’t be embarrassed. Be healthier and happier instead!
Are you dealing with fibroids or do you suspect you might be? Come ask questions and learn more from the Gennev Community forums!
I’m not a planner. Ask my team. It can drive them nuts; I tend to spring things on people as ideas come to mind.
I’m trying to take a different, more thoughtful approach in 2021. Especially as it comes to my emotional health.
Like so many people in the U.S., the events of the past week weigh heavy on my heart and have instilled an anger that I can’t shake. Plus my physical and emotional health have changed in the past 3 months. Perimenopause mental health and physical changes are no joke.
I eat pretty well as veggies, protein, and wine; run and walk most every day, and I’m expanding my movement to include yoga and a standing desk to help with achy hips and hamstrings.
But (gulp), it’s been five years since my last pap exam or mammogram. And now that I’m 47 and have a history of colorectal issues in my family, it’s the year of my first colonoscopy.
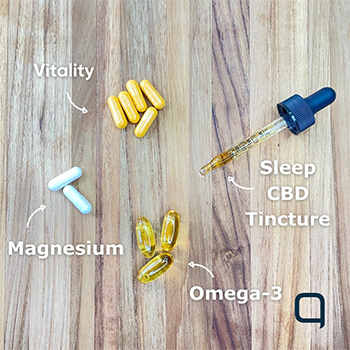
I audited my supplements as I take Gennev Vitality in the morning (I recommend taking it in the morning due to the high levels of B vitamins for energy) and the Multi-Tasker Magnesium before bed to help with sleep and anxiety. I also take Sleep CBD Tincture at bedtime to help me relax and fall asleep. It’s magical.
That’s my check-in. I hope you check in too.
Here’s my 2021 “take control of my health” plan:
Use my FSA funds. If I didn’t have the access to health coaches like I do being the Gennev CEO, I would spend on that service. I need an accountability partner to help with mindfulness and being more creative with my diet. Instead, I’ll spend it on an osteopath that helps with my aches and pains.
Yoga two times per week. I subscribed to the Peloton app, and I am committed to classes, even if I only have time for the 20-minute classes.
Pap exam and mammogram appointments are scheduled for February. I’m still working up the courage for the colonoscopy.
Dry January. I’m 10 days in and while I miss a glass of wine with dinner (and perhaps more), I feel clean without all the sugar.
Add Omega-3 and Vitamin D to my supplement routine. After speaking with Stasi Kasianchuk, Gennev’s Director of Health Coaching and my eye doctor, I’m adding Omega-3 for dry eye and Vitamin D for my bones. Bonus, it helps your immune system.
Protein! Amanda Thebe got me on to protein powder. I sprinkle it on my morning oatmeal.
In the past week, we’ve seen the volume of appointments with our doctors and health coaches spike. It’s apparent that many of you are starting 2021 with a focus on your health too. What’s most important is getting healthy and comfortable in the body that you have. Acceptance is medicine.
Do you have a “take control of my health” plan for 2021? If you do and you’re proud of it, send it to me. I’ll keep you accountable and will ask you to do the same for me.
And if you need help building your plan, set aside $45 and book an appointment with a coach. If you’re ready to take action, we’re here to help keep you accountable.
Here’s to a better week than the last,
Jill
Co-founder and CEO, Gennev
Getting out of bed can get tougher as we get older, and not just because our “to-do” the list is starting to look like a phone book. For the 27 million Americans with osteoarthritis and the 1.3 million with rheumatoid arthritis, getting out of bed can be an exercise in pain. Menopause joint pain fatigue and arthritis and are a real thing for many women, but there are some things that can be done.
Both rheumatoid arthritis (RA) and (OA) can develop or worsen in menopause, indicating that hormone levels play a role. What that role is exactly isn’t yet known as one theory is that estrogen may help reduce perception of pain. Whether or not menopause can actually cause RA or OA is still a matter of debate.
Because the cause(s) of arthritis and any correlation with menopause are still undetermined, there isn’t a cure, and treatment options are limited. However, this is one of those times when the choices we make can have a very big impact on our quality of life. We took the question of arthritis to our doctors of physical therapy, Meagan and Brianna.
I just got a diagnosis of arthritis. Is it time to upgrade my couch?
One of the biggest issues in managing arthritis isn’t the pain, our PTs tell us, it’s the notion that a diagnosis of arthritis means you need to slow down or stop all activity to preserve your joints from further damage.
Nope, says Bri. “Motion is lotion. Even if you have menopause arthritis symptoms, sitting still, not moving, is worse for your body than activity. People who get a diagnosis of arthritis or degenerative disc disease often fear that moving will make things worse. But activity and exercise that keep you stretching and moving are really important for maintaining flexibility and strength.”
But isn’t the arthritis pain telling me to stop?
There isn’t actually a correlation between the severity of the disease and the severity of pain, says Meagan. Someone with only mild degeneration can feel a lot of pain, whereas someone with bone-on-bone arthritis may not feel much at all; it depends on the individual. What that means to you is that even if it hurts, you’re probably not doing additional damage as and you may be doing some real good.
OK, so how do I exercise with arthritis in menopause?
A diagnosis of arthritis is scary, so a visit to a physical therapist might be your best next step. When fear of pain or doing damage means we start limiting ourselves, PTs can help us understand our true limitations and how to exercise safely.
Once you have the diagnosis, it’s time to make some good choices about managing the condition. A PT can help you”¦
Determine the right activity and level of activity. Arthritis presents differently in different people, Bri says, so your choice of activity depends on what works for you. For some, continuing with or even increasing their current activity is fine. For others, switching to non-weight-bearing such as pool or bicycle might be more comfortable.
Learn how to strengthen and stabilize joints. “The more stability a joint has, the less “slop and play’ there is in the system,” Meagan says. “That looseness and instability is what could pinch the meniscus in the knee, for example, or the cartilage, and further contribute to tissue break down. If you’ve got good stability and co-contraction when the joint is moving, you won’t have the wiggles and dings that end up causing additional damage. We can help you learn to build the supporting muscle around the joint that provide the stability and flexibility that allow the joint to function.”
Evaluate your true range of motion. “Seeing a PT for a formal evaluation is helpful,” says Meagan, “because a fearful person may start to restrict their range of motion. If the joint should have 90 degrees of range, but you limit that motion to just the middle 45 degrees, you’re overusing that portion of the joint surface. You need to share the load over the entire joint surface, the way it was designed. Wearing away at a portion of the joint can cause more problems over time.” PTs can help you understand not only the restriction you’re dealing with but also how you can begin extending that range safely.
Determine the true cause of pain. According to Bri, a PT can help determine if the pain you’re feeling is truly from the joint itself, or if it’s “referred” from somewhere else. Is it a muscle restriction or tight hip flexor? Or is it maybe a trigger point in a nearby muscle or a pinched nerve in your back? Identifying other sources of pain can be really helpful in determining a treatment plan.
Reduce pain. Ever heard of the “Gate Control Theory” of pain? It goes like this, Meagan says: the brain can really only accept one signal at a time, traveling up the peripheral nervous system from the limbs. Once a signal is received, it temporarily shuts the brain off from getting other messages, effectively “closing the gate.” Pain signals as while it may not seem like it when you stub your toe as travel relatively slowly. So if you can get another signal there first, it can shut the gate to pain, reducing our sensation of hurt. A PT can teach you ways to “wiggle” your joints to both shut the gate to pain but also to spread synovial fluid and lubricate sore joints.
What else can I do to manage my arthritis? Does post-menopausal arthritis go away?
Arthritis does seem to run in families. And it disproportionally affects post-menopausal women. Given that, it’s understandable that many women feel they’re likely doomed to decades of increasing pain and decreasing functionality.
However, say our PTs, there are so many factors that are within your control, that a diagnosis of arthritis doesn’t have to signal the end of your active life.
Stop smoking. Smoking makes arthritis worse. It may accelerate the destruction of cartilage or impede its repair. It reduces the effectiveness of treatments, complicates surgery, and increases mortality risk. If you can stop, do.
Maintain a healthy body weight. Smoking and BMI are tough topics for our PTs to broach with their patients, they tell us, but “I wouldn’t be doing my job well if I didn’t bring it up,” says Meagan. Bodyweight, like smoking, takes a toll on joints. Intermittent fasting during menopause and” losing even one pound can take four or five pounds of pressure off your knees with every step,” Meagan says. “That’s worth celebrating!”
How to keep arthritis from getting worse
Try topical remedies. Arnica, Biofreeze, even just using lotion for arthritis to touch and massage the painful area can help desensitize you to the pain, the PTs tell us.
Apply heat. Warm water soaks, Epsom salt baths, dipping painful fingers in warm paraffin wax as heat really helps lubricate the joints. “Think of putting maple syrup in the microwave,” Meagan says. “It gets nice and thin and runny and it covers more of your waffle. The same is true of synovial fluid and joints. You want it to coat the whole joint surface so it can lubricate the joint better.”
Stretch and move. “People really overlook the importance of stretching and moving,” says Bri. “If you’ve been on your computer for a while, take five minutes, do some forearm stretching, maybe find a quiet corner and do some foam rolling of hips and shoulders. If your fingers hurt, grab a couple of rubber bands, put them around your fingers, and open and close your hands. Get a soft ball to squeeze. These help build up strength and keep the joints in motion.”
Strengthen your core. This may seem like an odd remedy for pain in the wrist or shoulders or hands, but the stronger your core is, the less work your appendages have to do. “It’s that slop factor again,” Meagan tells us. “If your hips and abdomen and pelvis and lower back are strong, your knees and ankles don’t have to work as hard to correct for the weakness in the chain.” Although somewhat counterintuitive, a large part of the pain caused by a weak core is ultimately felt through pain in the knees for women in menopause.
Get good shock absorbers. Want to keep running? Get good shoes and/or inserts. The right shoes can stabilize and cushion, meaning less shock traveling up from the impact with the road. For cyclists, good gloves with the right padding can minimize impacts on your hands and up the chain from there.
Leverage the power of hydration and diet. It’s more effective than you might think, Bri tells us, you have to avoid a lot of foods in menopause as well as eat and drink the right things. Drink lots of water. Eat turmeric and other vitamins for menopause symptoms. Boost intake of anti-inflammatories and Omega-3s for women.
A diagnosis of arthritis isn’t the end of your active life; for most of us, it’s livable and manageable. “Too many people let a diagnosis of arthritis be an excuse to stop being active,” says Meagan, “but there are ways to have some control over the pain and the progression of the disease. A positive mindset and the decision not to let it victimize you are really powerful tools. Use them.”

Brianna

Meagan
Are you dealing with a diagnosis of arthritis? What are you doing to manage it? Please share what you’re doing and how well it’s working! Leave a comment below, on our Facebook page, or in our private Facebook group Midlife & Menopause Solutions.
Science is starting to uncover the many ways our gut flora affect our health. While many of us still believe the beneficial bacteria is good for digestion (and it is), it does a whole lot more.
Dr. Anna Garrett chats about the “Gut-Brain Axis”
In this podcast, metabolic surgeon and gut expert Dr. Erika La Vella talks with Gennev’s Director of Health Coaching Stasi Kasianchuk about the bi-directional relationship between your gut and your brain.
The “Gut-Brain Axis” affects your perception, cognition, your nervous system, your mood, pretty much everything. Given that, and how cattywampus everything can be during menopause anyway, doesn’t it make sense to be sure your gut is getting exactly what it needs?
This is why we bang on about nutrition here at Gennev “ it’s so important to feed yourself well, because it literally affects everything in your body. Good fiber helps the beneficial flora in your gut to thrive so it continues pulling nutrition from the food you eat and sending it where it does the most good.
Like virtually everything in nature, diversity is best, so eat lots and lots of veggies: 30 different kinds a week, according to Dr. La Vella. The more diverse your vegetable selection, full of vibrant colors and flavors, the better. Because different micronutrients have different functions in the body, “eating the rainbow” really does provide the most comprehensive care.
And if you can’t get them all, supplementation can help fill the gaps, so consider Gennev’s Vitality pack. Thirty veggies is a lot, and if that means you’re bumping up your fiber, you’ll want to take it slowly. While Dr. La Vella assures us that gas is normal and means your gut flora is doing their job, ramping up fiber too fast can cause more than ordinary gas!
TRANSCRIPT TO FOLLOW
Are you taking care of your microbiome? What do you do to keep those good bacteria healthy and thriving? We’d love for you to share your tips for eating the rainbow, getting good probiotics, protecting beneficial gut flora, etc., so please join the conversation on the Gennev Community forums!
Bring up menopause in friendly conversation, and the mood is likely to plummet. While you may find comfort in knowing that you’re not alone, talk turns quickly to the miserable experiences of menopause: breaking out in a visible sweat while in an important business meeting, waking up drenched at 3 a.m. and not being able to go back to sleep, gaining weight around your middle despite not changing your eating or exercise habits, or flying off the handle when your partner looks at you the wrong way. And many women continue to suffer since traditional care often leaves huge gaps in providing them the relief they need in menopause.
With predominantly negative images surrounding menopause, it may come as a surprise to find out that it’s possible to feel AMAZING during this stage of life. “You don’t have to suck it up and grin and bear it,” says Jill Angelo, founder of Gennev. “Ninety-four percent of our patients report an improvement in their symptoms as a result of working with Gennev providers. Our mission is to improve the standard of care for women in their post reproductive years. This can be a high point in women’s lives. Why allow menopause to hold them back? Let’s catapult them to what’s ahead.”
What is Integrated Menopause Care?
Gennev’s successful standard of care is Integrated Menopause Care, a team approach between you, a medical doctor, and a health coach. “Women need medical care and lifestyle change to manage their menopause,” says Angelo. “There’s no one prescription pill that can do it all. There’s no one vitamin or behavior change that can do it all. It’s the two working together that makes menopause symptoms manageable.”
On the medical care side are Gennev’s doctors, who are board-certified ob/gyns with experience in treating women in menopause. Many are also certified by the North American Menopause Society as menopause practitioners or are working on their certification. They also follow Gennev’s evidence-based protocols for treatment.
To help women make the necessary lifestyle changes that support their health during their post-reproductive years, Gennev has a team of health coaches who are registered dietitians and often use cognitive behavioral therapy approaches when appropriate. They guide women to create plans and set goals in nutrition, fitness, sleep, mindfulness, and stress management. Then, they help them implement those plans and provide accountability and support so women can achieve their goals, feel better, and live longer, healthier lives. All of the coaches have training and experience working with women in menopause, in addition to following Gennev’s protocols, working in lockstep with Gennev’s doctors.
“It’s truly a care team approach,” says Rebecca Dunsmoor-Su, M.D., the chief medical officer for Gennev. “Every woman’s menopause journey is as unique as she is, so the best treatment for menopause for her will generally require a little experimentation and tweaking to get just the right formula. The care team works together, keeping each other apprised of what’s going on, so a woman doesn’t have to worry about updating her providers.”
What makes Gennev’s Integrated Menopause Care approach different?
Gennev offers a multi-level, in-depth, personal approach compared to traditional menopause care. Most women go to their primary care physician or ob/gyn when menopause symptoms start. Unfortunately, in traditional settings, few doctors are trained in menopause care, and women can end up with multiple medications, general advice, and even misinformation. “Women often leave appointments feeling dismissed and frustrated, as well as with prescriptions that are just addressing the symptoms and not dealing with what’s at the core, which is hormonal change,” says Angelo. Treating the whole person is the only way to improve a woman’s quality of life versus just band-aiding the symptoms.”
This model draws from the broader definition of Integrated Care as defined by the NHS as, “Integrated care is an organizing principle for care delivery with the aim of achieving improved patient care through better coordination of services provided. Integration is the combined set of methods, processes, and models that seek to bring about this improved coordination of care.”
The whole-person approach
Estrogen affects more than just your reproductive system, which is why the symptoms of menopause are so widespread. Estrogen receptors are found throughout a women’s body, causing this hormone to affect nearly every system in the body, from bones and muscles to the heart and brain. “Because of hormonal shifts during menopause, this is the one time in your life when certain things will set off other things,” says Dr. Dunsmoor-Su. “If a woman’s not sleeping well, it also correlates with her gaining weight because you gain weight when you don’t sleep well.” The effects also go beyond physical health. They affect women mentally and emotionally. In addition, how you manage the changes that are happening now impacts your health down the road.
“When you think of a women’s health, post reproductively, it starts with menopause, and menopause frames up your long-term chronic health,” says Angelo. “Until now, women were never educated on how taking care of our menopausal symptoms also has preventive aspects for our long-term chronic care when we’re in our 50s, 60s, 70s, specifically to heart disease, diabetes, osteoporosis, Alzheimer’s disease, and dementia.”
With all of that at stake, it’s even more critical to ensure that you’re receiving integrated menopause care. Unfortunately, even major organizations like the American Medical Association and the American College of Obstetrics and Gynecology provide little support in menopause, making it hard to find this type of care. That’s why Gennev created its telehealth approach so no matter where you live in the United States, you have access to a menopause specialist.
Physical exam not required
Menopause isn’t diagnosed by a physical exam or blood test. Menopause is the point when you’ve gone an entire year without menstruating–the one-year anniversary of your last period. Likewise, there’s no definitive way to determine where you are in perimenopause, the transition to menopause, or how long it will last (typically four to 10 years).
Despite expensive diagnostics, including hormone level tests, or multiple prescription medications, many women continue to suffer. Quality menopause care starts with a conversation. Menopause-trained doctors know the right questions to ask, and at Gennev, our doctors have the time to really listen to you and understand what you’re going through. Unlike traditional doctor appointments, where you get only 10 to 15 minutes with your doctor, your initial appointment with a Gennev doctor will be 30 minutes. And then, your care continues with follow-up visits and recurring appointments with a health coach.
How one woman found relief from menopause symptoms
“Everything started going haywire about a year ago,” says Kristine, 50, a Seattle-based realtor. “I was waking up three to four times a night with night sweats. I was fuzzy during the day. My body started changing shape, and I was gaining weight in my middle area even though I was exercising more. My anxiety was out of control. It was affecting my mental health as well. And the thinning hair and drier skin, I felt like I was aging at a rapid pace.”
Kristine tried all of the usual routes to find relief. Her mom wasn’t any help; she had very few, if any, symptoms. Her much younger doctor, who’s a nurse practitioner and naturopath, had little experience with menopause. While she offered suggestions, including prescribing bio-identical hormones, nothing helped. “I got very frustrated with the whole process,” she says.
When she finally started talking to her girlfriends about her symptoms, one of them suggested Gennev, a company focused on helping women through this transition. “It was the specialty I really needed,” says Kristine, who has had two doctor appointments and two health coach appointments in the time it would have taken her to see her regular doctor.
The next level of care
Kristine’s virtual appointment with one of the Gennev doctors couldn’t have been better. “She was confident that we could get this under control, which was such a relief for me,” she says. “She knew her stuff inside and out.” Even though Kristine prefers to avoid medications in favor of natural remedies, she agreed with the doctor’s recommendation to try an estrogen patch. “My symptoms were so severe that I just couldn’t keep living the way I was,” Kristine says. “We talked through my concerns, and I felt comfortable going that route.”
Within about a week, all of Kristine’s menopause symptoms were subsiding. “Everything is moving in the right direction,” she says. But her care didn’t stop there. She started to meet regularly with one of Gennev’s health coaches who’s helped her implement healthy new behaviors into her life like meal planning, eating more protein, and lifting weights. “I learned that women lose muscle mass as they get older, so putting on muscle is now my goal,” says Kristine, who is impressed with the quality of care that she’s getting at a price that’s less than what many of her friends pay for coaching. “Recently, we had an appointment on a Thursday and over the weekend my health coach checked in and sent links for meal prep and recipes for high-protein snacks. It feels like she cares and has a vested interest in my success. It feels like it’s the next level of care.”
In the amount of time Kristine would have been suffering, waiting for an appointment with her regular doctor, she thrived. “I’m not waking up at all in the middle of the night. My anxiety is way down. I’m feeling stronger. My clothes are fitting better. It has been life-changing,” she says.
How to get started with Gennev Integrated Menopause Care
While Kristine’s journey to feeling better started with a friend’s referral, you can begin your journey now to finding relief from your menopause.
It starts with a simple intake or quiz we call the Menopause Assessment. It provides you with personal health insights about where you’re at in menopause. It also sets up your initial visit with a Gennev doctor, providing information essential for diagnosis, medical guidance, and prescription support.
The next step is to meet with a Gennev health coach to implement a lifestyle plan based on health concerns you shared in your Menopause Assessment and with your doctor. The plan often includes nutrition, movement, mindfulness and stress-relief tactics, and sleep practices to address your personal situation.
As the weeks go by, you control how often you connect with your health coach”whether via appointment or text messaging. She is there as an accountability partner and supporter for you as long as you need her. And if you need to see the doctor months down the road”to check in on a prescription or to report changes in your symptoms”your coach can help you decide when that moment is right for you.
That’s the power of integrated care, and Gennev is bringing this proven approach to treating menopausal symptoms. “Let’s get you feeling better and improving your quality of life now so that you can function and thrive in life, and at the same time, prevent long-term chronic illness,” Angelo says.
It’s time to experience Gennev’s proven integrated care model for menopause. Get started by scheduling an appointment today.
In Japan and China, they call it “fifties shoulder” because it’s a common symptom among women in menopause and midlife. In the west, it’s generally referred to as “frozen shoulder,” and among health care professionals, “adhesive capsulitis.”
By whatever name, a frozen shoulder is painful and limiting. So let’s talk about what it is, why it happens, and how to find relief.
What is frozen shoulder?
Frozen shoulder is inflammation in the connective tissue of the “head” of your shoulder, the “shoulder capsule.” Over time, the tissue of the joint gets thicker and tighter, and adhesive bands of tissue can form in the joint. Full range of motion (particularly reaching over your head or behind your back) becomes more and more painful until finally it’s all but impossible.
Many sufferers say it happens in three stages: stiffening (or painful), frozen, thawing. The good news is, it can thaw, and with the right treatment and therapy, most sufferers can regain their full (or nearly full) range of motion, and eliminate or greatly reduce the pain.
Why does it happen and who’s at risk?
We don’t entirely know why frozen shoulder happens. Sometimes it flares up all on its own, sometimes it may be the result of an earlier injury.
Frozen shoulder can also be hard to diagnose, since it’s generally identified by process of elimination (determining what it’s not, like a rotator cuff injury). Lots of folks let it go, believing it to be arthritis, but please don’t do that: it’s not arthritis, and because frozen shoulder is progressive, the sooner you catch it, the less you’ll suffer and the better the long-term prognosis.
The condition happens to around 3% of the population, most often in adults 40–65, and more commonly to women than men. It’s also more common among people with diabetes. It may happen so frequently in menopause because women lose the inflammation-dampening benefits of estrogen.
Another possible explanation for frozen shoulder is our emotions and the body posture that results from those emotions. Says Jennifer Mason, acupuncturist and owner of Vitamin Chi: “Maybe you tighten up your back or roll your shoulders forward when you’re feeling defensive. A gentle noticing of how you hold your body and what makes you tense up can help here.”
How can I prevent or treat frozen shoulder?
Frozen shoulder can’t really be prevented unless you’ve suffered an injury to the shoulder that makes movement difficult. In that case, consult a doctor for advice on exercises that will keep the shoulder mobile.
If you’re already experiencing some stiffening and/or pain, don’t wait to get help.
Traditional therapies usually start with taking NSAIDs (anti-inflammatories like aspirin or ibuprofen), alternating ice and heat on the affected area, gentle stretching, and corticosteroid injections in the joint. Your doctor will likely suggest that you work with a physical therapist to slowly increase flexibility until the shoulder returns to normal. In some cases, surgery is an option: the two types are manipulation that stretches the tissue, and arthroscopy, which cuts through the tight tissues.
Non-surgical treatment options for frozen shoulder
In addition to those therapies for frozen shoulder, there are other steps that might help relieve pain and increase motion. Here’s what Jennifer Mason suggests:
- Get an assessment of your posture. As Jennifer says, in this modern day, we’ve “lost sense of what ‘straight’ is.” If, like many of us, you hunch over a keyboard at a desk all day, you may be suffering from Upper Cross Syndrome, a lengthening and weakening of the spine and back muscles and shortening of chest muscles (pecs). This rounding forward of the shoulders pulls the upper body out of balance and can contribute to the pain and loss of motion.
- Get expert help to release trigger points in the subclavius and pectoralis minor. Jennifer suggests the Trigger Point Therapy Workbook or The Frozen Shoulder Workbook which features treatments just for frozen shoulder. Written for laypeople, it has “far less medical jargon,” which, in my very lay opinion, is always a bonus.
- Healthy blood circulation helps healing, so don’t forget the heat and exercise (and cupping and acupuncture). Says Jennifer, “I also have a liniment that I like to use for sore muscles—wan hua oil or the “pain terminator.'”
- Jennifer also advocates “circulation-promoting herbal formulas” but says you should consult a qualified health care professional before taking these, as some formulas have blood-thinning properties. CBD is another treatment that has helped many women in similar situations, and could be worth looking into.
The majority of frozen shoulder cases resolve in time, but it can take up to three years to recover. Taking the right steps sooner rather than later can decrease the pain and duration of the condition and increase your chances of getting full usability back.
Something to bear in mind: while we do not recommend delaying treatment, we also know it’s a real world out there. Some insurance companies do not cover treatments for frozen shoulder, or may not cover it completely. Because the disease often resolves over time, your insurance agency may insist that you “wait it out” rather than get treatment. So it’s good to check before proceeding, and frankly, to advocate for coverage if you’re told to grit your way through it. Women have compared the pain of frozen shoulder to childbirth, only it lasts a whole lot longer and doesn’t result in a baby.
We can help you get the care you need
- Meet with a Gennev Doctor – If you are experiencing frozen shoulder, a board-certified gynecologist/menopause specialist can give you a trusted opinion, determine if medication is right for you, and provide prescription support.
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
Our environment can be pretty heavy with things that are bad for our health, including endocrine-disrupting substances.
An Important conversation with Mary Purdy
Cleansers, detergents, scrubs, things we use to clean our environments and ourselves may be doing more damage to our health than than they prevent. What about products that go on and in our bodies “ soaps, creams, powders, makeup, body wash, deodorants and anti-perspirants, hair sprays, plastic containers to hold our food in the fridge or microwave. How many products do you come in contact with every day, all days of your life?
And it’s not just the products we use. Disruptive chemicals can be in our clothes or furniture or daily use objects as fire-retardants or easy-clean surfaces.
Mary Purdy is an expert on helping us minimize our exposure to toxins in our environment and maximize our efficiency in ridding them from our bodies, homes, and workplaces.
TRANSCRIPT TO FOLLOW
So, you took a menopause test after dealing with various symptoms and you found out you may be indeed going through menopause. What now?
Well, search on the word “menopause” on the Internet, and where once there was mostly silence, crickets chirping, and the distant sound of an eagle’s cry, now there’s “¦ a lot.
Menopause is having its day, and while that is very good and very overdue, it can be hard to wade through the chaos and separate good information on menopause treatments from rumor and hyperbole. We’ll help you cut through the noise and understand the best menopause treatment options available to you.
If you are looking for treatment options, a Gennev menopause-certified gynecologist can give you a trusted opinion, determine if medication is right for you, and they can provide prescription support. Book an appointment with a doctor here.
Menopause Treatment Guidelines
Menopause is a natural and normal part of a woman’s life, I hear you say. Do we really need treatments for it?
Those lucky few who fly through menopause with nary a hot flash may not need any kind of external support. But many really suffer with menopause vaginal issues, itching, sleepless nights, joint pains, annoying hot flashes, anxiety risks, brain fog, and a host of symptoms that range from disruptive to crippling.
Fortunately, there are treatments and behaviors that can help relieve menopause symptoms, so let’s talk about which menopause treatments work and which don’t, what’s safe and what isn’t.
How can menopause be treated?
At Gennev, we’ve found that menopause treatment follows three general tracks: medical intervention (hormone replacement, antidepressants, etc.), lifestyle and behavioral adaptations (diet, exercise, supplements, alternative therapies), or some combination of the two.
Every woman’s menopause journey is as unique as she is, so the best treatment for menopause for her will generally require a little experimentation and tweaking to get just the right formula.
Medical treatments for menopause
For many women, the safest and most effective menopause treatment is hormone replacement for hot flashes or HRT. While the poorly conducted Women’s Health Initiative trial appeared to indicate that HRT was not safe, the truth is that for most women, if taken correctly, HRT is safe and the best treatment for menopause symptoms.
HRT is the most universally effective treatment for hot flashes and vaginal dryness. In addition, it may provide protection against osteoporosis, heart disease, and even Alzheimer’s disease, so the long-term effects need to be brought in to the risk-benefit analysis.
HRT replaces what your body no longer makes enough of: estrogen. Estrogen does not appear to cause breast cancer (if it did, wouldn’t every woman have it?). However, since it appears to stimulate existant estrogen-sensitive breast cancer, it’s not recommended for women who’ve already had this type of cancer.
Birth control pills and hormonal IUDs help many women with symptoms of perimenopause and menopause. Again, birth control pills or a hormonal IUD like Mirena are not good options for women with a history of estrogen-sensitive cancers, but for many women, the steady release of estrogen can really help balance out hormones during the usually tumultuous perimenopause years.
Antidepressants in low doses can help relieve hot flashes and are generally safe for women regardless of breast cancer risk. The antidepressant dosage recommended for hot flashes is lower than the dose typically used to combat depression.
Moderate vaginal dryness, lichen sclerosus (different than MS), and moderate incontinence can be successfully treated in many women with laser treatments like the Mona Lisa Touch. This is a good, non-hormonal treatment, but it hasn’t been approved by the FDA (though it has been “cleared”). Be sure the practitioner is well-trained in its use and capabilities, and be aware that it is often not covered by insurance.
Bio-identical progesterone creams from a compounding pharmacy are tricky. These are unregulated, so we don’t recommend their use. Additionally, they are no more “natural” than the FDA-regulated medications.
Menopause medicine: over the counter treatments
Taking OTC medicines for menopause can be a bit concerning because lack of oversight from the FDA can mean some products can’t be safely verified. Taking ibuprofen for cramps or to reduce heavy bleeding, or fiber supplements for women’s constipation is probably just fine; getting non-regulated bio-identical hormones from a compounding pharmacy or from the Internet may not be. If you’re going with hormones, please get a prescription from your GP or OB/GYN.
Over-the-counter medications are by nature less powerful than their by-prescription siblings, so you may not find complete or sustained relief. If you’re really suffering, there’s no reason not to get in touch with a menopause doctor near you and get a prescription.
If you have any concerns about your medication, OTC or other, check with your GP, OB/GYN or one of our menopause-specialist telemed doctors.
Natural menopause treatments that really work
First, it’s important to define “natural.” Some define it as “not from Big Pharma.” We understand why women prefer a more natural alternative, but (1) “natural” is not well-defined by any authoritative, regulating body like the FDA, and (2) “natural” does not mean “safe.” Death cap mushrooms are natural, but I wouldn’t want one in my salad.
There are natural remedies that appear to help women, but not enough studies have been done to verify their efficacy. Our approach is, if it doesn’t hurt, and it might be able to help, it’s worth a try. Check out our thoughts on natural remedies in our article “Hot flashes and alternative therapes: What really works?”
Soy (in food, not concentrated supplements, for hot flashes), black cohosh (for hot flashes), Omega 3 (for brain fog and fatigue), vitamin E (for hot flashes), and magnesium glycinate (joint pain, anxiety, and sleep) are all safe and reasonable things to try for menopause symptoms. And any supplement in the Gennev shop has been tested and made to rigorous standards.
Just remember, if you’re adding any concentrated substance to your diet (and this includes supplements, capsules, analgesics, etc.), please check with a doctor who knows your history and what medications you’re on, just to be sure there’s no concern about interactions.
Behaviors and menopause alternative treatments for symptoms
If you’re uncomfortable with hormones or unable to take them, you’re not out of luck. Behavior changes can take you a long way.
Most of these are things you know or can guess; the difficulty is in sticking with them long enough to see real results.
Hydration is so important and will help you more than you can imagine. Your body holds less water now, so dry skin, dry eyes, headaches, fatigue, and brain fog in menopause can all be helped by drinking more. Check out the book Quench by Dana Cohen, MD, if you need more encouragement to hydrate!
Exercise is critical.
Impact exercise like running and walking can help with bones. Building muscles after forty as well as upper body strength can help with retaining muscle and increasing resting metabolism. Core strength can help with balance, meaning fewer falls. And all of these can help lift mood and invite better sleep.
Diet
Diet is another area where a few tweaks can make a significant difference. Now is when you need to increase lean protein and boost healthy greens. The Mediterranean diet is particularly beneficial for women with its emphasis on heart-healthy greens and grains and de-emphasis on red meats. Your brain will benefit, your bones will benefit, and as we age into higher risk of diabetes and heart disease, you’ll have a head start on avoiding long-term illness.
Sleep hygiene
Sleep hygiene is a good idea for everyone, but it’s particularly helpful for peri- and post-menopausal women. Setting a bedtime routine, optimizing your bedroom for sleep, banishing screens two hours before bedtime, going to bed and getting up at the same time every day “ you can start to train your body and mind to understand sleep signals so you can get better rest.
Stress reduction strategies
Don’t just say “yeah yeah” and wave vaguely at the piles of laundry, the bulging work email inbox, the kids, the dog, etc. Yes, life is busy and stressful. No, it’s not healthy, and you need to acknowledge when you need help and a lightening of the load. Taking time for self-care isn’t indulgent or decadent “ it’s critical to good mental and physical health.
If you’re challenged or confused about any of these, or just need an accountability partner, we strongly suggest you sign up for Gennev’s Health Fix. You’ll get unlimited access to our Health Coaches, all of whom are Registered Dietitian Nutritionists and have had special training in menopause care.
There are menopause treatments that really work. It may take some adding, subtracting, tweaking, and testing, but most women find some combination of medical intervention, alternative treatments, and lifestyle change makes them feel a whole lot better.
To find out what route is truly the safest and most effective for you and the menopause symptoms you’re dealing with, talk with a menopause specialist physician. Team up with a Health Coach for ideas and accountability. What’s happening in your body may be frustrating, but it’s normal, and you’re not alone on this journey.