Science is starting to uncover the many ways our gut flora affect our health. While many of us still believe the beneficial bacteria is good for digestion (and it is), it does a whole lot more.
Dr. Anna Garrett chats about the “Gut-Brain Axis”
In this podcast, metabolic surgeon and gut expert Dr. Erika La Vella talks with Gennev’s Director of Health Coaching Stasi Kasianchuk about the bi-directional relationship between your gut and your brain.
The “Gut-Brain Axis” affects your perception, cognition, your nervous system, your mood, pretty much everything. Given that, and how cattywampus everything can be during menopause anyway, doesn’t it make sense to be sure your gut is getting exactly what it needs?
This is why we bang on about nutrition here at Gennev “ it’s so important to feed yourself well, because it literally affects everything in your body. Good fiber helps the beneficial flora in your gut to thrive so it continues pulling nutrition from the food you eat and sending it where it does the most good.
Like virtually everything in nature, diversity is best, so eat lots and lots of veggies: 30 different kinds a week, according to Dr. La Vella. The more diverse your vegetable selection, full of vibrant colors and flavors, the better. Because different micronutrients have different functions in the body, “eating the rainbow” really does provide the most comprehensive care.
And if you can’t get them all, supplementation can help fill the gaps, so consider Gennev’s Vitality pack. Thirty veggies is a lot, and if that means you’re bumping up your fiber, you’ll want to take it slowly. While Dr. La Vella assures us that gas is normal and means your gut flora is doing their job, ramping up fiber too fast can cause more than ordinary gas!
TRANSCRIPT TO FOLLOW
Are you taking care of your microbiome? What do you do to keep those good bacteria healthy and thriving? We’d love for you to share your tips for eating the rainbow, getting good probiotics, protecting beneficial gut flora, etc., so please join the conversation on the Gennev Community forums!
Bring up menopause in friendly conversation, and the mood is likely to plummet. While you may find comfort in knowing that you’re not alone, talk turns quickly to the miserable experiences of menopause: breaking out in a visible sweat while in an important business meeting, waking up drenched at 3 a.m. and not being able to go back to sleep, gaining weight around your middle despite not changing your eating or exercise habits, or flying off the handle when your partner looks at you the wrong way. And many women continue to suffer since traditional care often leaves huge gaps in providing them the relief they need in menopause.
With predominantly negative images surrounding menopause, it may come as a surprise to find out that it’s possible to feel AMAZING during this stage of life. “You don’t have to suck it up and grin and bear it,” says Jill Angelo, founder of Gennev. “Ninety-four percent of our patients report an improvement in their symptoms as a result of working with Gennev providers. Our mission is to improve the standard of care for women in their post reproductive years. This can be a high point in women’s lives. Why allow menopause to hold them back? Let’s catapult them to what’s ahead.”
What is Integrated Menopause Care?
Gennev’s successful standard of care is Integrated Menopause Care, a team approach between you, a medical doctor, and a health coach. “Women need medical care and lifestyle change to manage their menopause,” says Angelo. “There’s no one prescription pill that can do it all. There’s no one vitamin or behavior change that can do it all. It’s the two working together that makes menopause symptoms manageable.”
On the medical care side are Gennev’s doctors, who are board-certified ob/gyns with experience in treating women in menopause. Many are also certified by the North American Menopause Society as menopause practitioners or are working on their certification. They also follow Gennev’s evidence-based protocols for treatment.
To help women make the necessary lifestyle changes that support their health during their post-reproductive years, Gennev has a team of health coaches who are registered dietitians and often use cognitive behavioral therapy approaches when appropriate. They guide women to create plans and set goals in nutrition, fitness, sleep, mindfulness, and stress management. Then, they help them implement those plans and provide accountability and support so women can achieve their goals, feel better, and live longer, healthier lives. All of the coaches have training and experience working with women in menopause, in addition to following Gennev’s protocols, working in lockstep with Gennev’s doctors.
“It’s truly a care team approach,” says Rebecca Dunsmoor-Su, M.D., the chief medical officer for Gennev. “Every woman’s menopause journey is as unique as she is, so the best treatment for menopause for her will generally require a little experimentation and tweaking to get just the right formula. The care team works together, keeping each other apprised of what’s going on, so a woman doesn’t have to worry about updating her providers.”
What makes Gennev’s Integrated Menopause Care approach different?
Gennev offers a multi-level, in-depth, personal approach compared to traditional menopause care. Most women go to their primary care physician or ob/gyn when menopause symptoms start. Unfortunately, in traditional settings, few doctors are trained in menopause care, and women can end up with multiple medications, general advice, and even misinformation. “Women often leave appointments feeling dismissed and frustrated, as well as with prescriptions that are just addressing the symptoms and not dealing with what’s at the core, which is hormonal change,” says Angelo. Treating the whole person is the only way to improve a woman’s quality of life versus just band-aiding the symptoms.”
This model draws from the broader definition of Integrated Care as defined by the NHS as, “Integrated care is an organizing principle for care delivery with the aim of achieving improved patient care through better coordination of services provided. Integration is the combined set of methods, processes, and models that seek to bring about this improved coordination of care.”
The whole-person approach
Estrogen affects more than just your reproductive system, which is why the symptoms of menopause are so widespread. Estrogen receptors are found throughout a women’s body, causing this hormone to affect nearly every system in the body, from bones and muscles to the heart and brain. “Because of hormonal shifts during menopause, this is the one time in your life when certain things will set off other things,” says Dr. Dunsmoor-Su. “If a woman’s not sleeping well, it also correlates with her gaining weight because you gain weight when you don’t sleep well.” The effects also go beyond physical health. They affect women mentally and emotionally. In addition, how you manage the changes that are happening now impacts your health down the road.
“When you think of a women’s health, post reproductively, it starts with menopause, and menopause frames up your long-term chronic health,” says Angelo. “Until now, women were never educated on how taking care of our menopausal symptoms also has preventive aspects for our long-term chronic care when we’re in our 50s, 60s, 70s, specifically to heart disease, diabetes, osteoporosis, Alzheimer’s disease, and dementia.”
With all of that at stake, it’s even more critical to ensure that you’re receiving integrated menopause care. Unfortunately, even major organizations like the American Medical Association and the American College of Obstetrics and Gynecology provide little support in menopause, making it hard to find this type of care. That’s why Gennev created its telehealth approach so no matter where you live in the United States, you have access to a menopause specialist.
Physical exam not required
Menopause isn’t diagnosed by a physical exam or blood test. Menopause is the point when you’ve gone an entire year without menstruating–the one-year anniversary of your last period. Likewise, there’s no definitive way to determine where you are in perimenopause, the transition to menopause, or how long it will last (typically four to 10 years).
Despite expensive diagnostics, including hormone level tests, or multiple prescription medications, many women continue to suffer. Quality menopause care starts with a conversation. Menopause-trained doctors know the right questions to ask, and at Gennev, our doctors have the time to really listen to you and understand what you’re going through. Unlike traditional doctor appointments, where you get only 10 to 15 minutes with your doctor, your initial appointment with a Gennev doctor will be 30 minutes. And then, your care continues with follow-up visits and recurring appointments with a health coach.
How one woman found relief from menopause symptoms
“Everything started going haywire about a year ago,” says Kristine, 50, a Seattle-based realtor. “I was waking up three to four times a night with night sweats. I was fuzzy during the day. My body started changing shape, and I was gaining weight in my middle area even though I was exercising more. My anxiety was out of control. It was affecting my mental health as well. And the thinning hair and drier skin, I felt like I was aging at a rapid pace.”
Kristine tried all of the usual routes to find relief. Her mom wasn’t any help; she had very few, if any, symptoms. Her much younger doctor, who’s a nurse practitioner and naturopath, had little experience with menopause. While she offered suggestions, including prescribing bio-identical hormones, nothing helped. “I got very frustrated with the whole process,” she says.
When she finally started talking to her girlfriends about her symptoms, one of them suggested Gennev, a company focused on helping women through this transition. “It was the specialty I really needed,” says Kristine, who has had two doctor appointments and two health coach appointments in the time it would have taken her to see her regular doctor.
The next level of care
Kristine’s virtual appointment with one of the Gennev doctors couldn’t have been better. “She was confident that we could get this under control, which was such a relief for me,” she says. “She knew her stuff inside and out.” Even though Kristine prefers to avoid medications in favor of natural remedies, she agreed with the doctor’s recommendation to try an estrogen patch. “My symptoms were so severe that I just couldn’t keep living the way I was,” Kristine says. “We talked through my concerns, and I felt comfortable going that route.”
Within about a week, all of Kristine’s menopause symptoms were subsiding. “Everything is moving in the right direction,” she says. But her care didn’t stop there. She started to meet regularly with one of Gennev’s health coaches who’s helped her implement healthy new behaviors into her life like meal planning, eating more protein, and lifting weights. “I learned that women lose muscle mass as they get older, so putting on muscle is now my goal,” says Kristine, who is impressed with the quality of care that she’s getting at a price that’s less than what many of her friends pay for coaching. “Recently, we had an appointment on a Thursday and over the weekend my health coach checked in and sent links for meal prep and recipes for high-protein snacks. It feels like she cares and has a vested interest in my success. It feels like it’s the next level of care.”
In the amount of time Kristine would have been suffering, waiting for an appointment with her regular doctor, she thrived. “I’m not waking up at all in the middle of the night. My anxiety is way down. I’m feeling stronger. My clothes are fitting better. It has been life-changing,” she says.
How to get started with Gennev Integrated Menopause Care
While Kristine’s journey to feeling better started with a friend’s referral, you can begin your journey now to finding relief from your menopause.
It starts with a simple intake or quiz we call the Menopause Assessment. It provides you with personal health insights about where you’re at in menopause. It also sets up your initial visit with a Gennev doctor, providing information essential for diagnosis, medical guidance, and prescription support.
The next step is to meet with a Gennev health coach to implement a lifestyle plan based on health concerns you shared in your Menopause Assessment and with your doctor. The plan often includes nutrition, movement, mindfulness and stress-relief tactics, and sleep practices to address your personal situation.
As the weeks go by, you control how often you connect with your health coach”whether via appointment or text messaging. She is there as an accountability partner and supporter for you as long as you need her. And if you need to see the doctor months down the road”to check in on a prescription or to report changes in your symptoms”your coach can help you decide when that moment is right for you.
That’s the power of integrated care, and Gennev is bringing this proven approach to treating menopausal symptoms. “Let’s get you feeling better and improving your quality of life now so that you can function and thrive in life, and at the same time, prevent long-term chronic illness,” Angelo says.
It’s time to experience Gennev’s proven integrated care model for menopause. Get started by scheduling an appointment today.
In Japan and China, they call it “fifties shoulder” because it’s a common symptom among women in menopause and midlife. In the west, it’s generally referred to as “frozen shoulder,” and among health care professionals, “adhesive capsulitis.”
By whatever name, a frozen shoulder is painful and limiting. So let’s talk about what it is, why it happens, and how to find relief.
What is frozen shoulder?
Frozen shoulder is inflammation in the connective tissue of the “head” of your shoulder, the “shoulder capsule.” Over time, the tissue of the joint gets thicker and tighter, and adhesive bands of tissue can form in the joint. Full range of motion (particularly reaching over your head or behind your back) becomes more and more painful until finally it’s all but impossible.
Many sufferers say it happens in three stages: stiffening (or painful), frozen, thawing. The good news is, it can thaw, and with the right treatment and therapy, most sufferers can regain their full (or nearly full) range of motion, and eliminate or greatly reduce the pain.
Why does it happen and who’s at risk?
We don’t entirely know why frozen shoulder happens. Sometimes it flares up all on its own, sometimes it may be the result of an earlier injury.
Frozen shoulder can also be hard to diagnose, since it’s generally identified by process of elimination (determining what it’s not, like a rotator cuff injury). Lots of folks let it go, believing it to be arthritis, but please don’t do that: it’s not arthritis, and because frozen shoulder is progressive, the sooner you catch it, the less you’ll suffer and the better the long-term prognosis.
The condition happens to around 3% of the population, most often in adults 40–65, and more commonly to women than men. It’s also more common among people with diabetes. It may happen so frequently in menopause because women lose the inflammation-dampening benefits of estrogen.
Another possible explanation for frozen shoulder is our emotions and the body posture that results from those emotions. Says Jennifer Mason, acupuncturist and owner of Vitamin Chi: “Maybe you tighten up your back or roll your shoulders forward when you’re feeling defensive. A gentle noticing of how you hold your body and what makes you tense up can help here.”
How can I prevent or treat frozen shoulder?
Frozen shoulder can’t really be prevented unless you’ve suffered an injury to the shoulder that makes movement difficult. In that case, consult a doctor for advice on exercises that will keep the shoulder mobile.
If you’re already experiencing some stiffening and/or pain, don’t wait to get help.
Traditional therapies usually start with taking NSAIDs (anti-inflammatories like aspirin or ibuprofen), alternating ice and heat on the affected area, gentle stretching, and corticosteroid injections in the joint. Your doctor will likely suggest that you work with a physical therapist to slowly increase flexibility until the shoulder returns to normal. In some cases, surgery is an option: the two types are manipulation that stretches the tissue, and arthroscopy, which cuts through the tight tissues.
Non-surgical treatment options for frozen shoulder
In addition to those therapies for frozen shoulder, there are other steps that might help relieve pain and increase motion. Here’s what Jennifer Mason suggests:
- Get an assessment of your posture. As Jennifer says, in this modern day, we’ve “lost sense of what ‘straight’ is.” If, like many of us, you hunch over a keyboard at a desk all day, you may be suffering from Upper Cross Syndrome, a lengthening and weakening of the spine and back muscles and shortening of chest muscles (pecs). This rounding forward of the shoulders pulls the upper body out of balance and can contribute to the pain and loss of motion.
- Get expert help to release trigger points in the subclavius and pectoralis minor. Jennifer suggests the Trigger Point Therapy Workbook or The Frozen Shoulder Workbook which features treatments just for frozen shoulder. Written for laypeople, it has “far less medical jargon,” which, in my very lay opinion, is always a bonus.
- Healthy blood circulation helps healing, so don’t forget the heat and exercise (and cupping and acupuncture). Says Jennifer, “I also have a liniment that I like to use for sore muscles—wan hua oil or the “pain terminator.'”
- Jennifer also advocates “circulation-promoting herbal formulas” but says you should consult a qualified health care professional before taking these, as some formulas have blood-thinning properties. CBD is another treatment that has helped many women in similar situations, and could be worth looking into.
The majority of frozen shoulder cases resolve in time, but it can take up to three years to recover. Taking the right steps sooner rather than later can decrease the pain and duration of the condition and increase your chances of getting full usability back.
Something to bear in mind: while we do not recommend delaying treatment, we also know it’s a real world out there. Some insurance companies do not cover treatments for frozen shoulder, or may not cover it completely. Because the disease often resolves over time, your insurance agency may insist that you “wait it out” rather than get treatment. So it’s good to check before proceeding, and frankly, to advocate for coverage if you’re told to grit your way through it. Women have compared the pain of frozen shoulder to childbirth, only it lasts a whole lot longer and doesn’t result in a baby.
We can help you get the care you need
- Meet with a Gennev Doctor – If you are experiencing frozen shoulder, a board-certified gynecologist/menopause specialist can give you a trusted opinion, determine if medication is right for you, and provide prescription support.
The information on the Gennev site is never meant to replace the care of a qualified medical professional. Hormonal shifts throughout menopause can prompt a lot of changes in your body, and simply assuming something is “just menopause” can leave you vulnerable to other possible causes. Always consult with your physician or schedule an appointment with one of Gennev’s telemedicine doctors before beginning any new treatment or therapy.
Our environment can be pretty heavy with things that are bad for our health, including endocrine-disrupting substances.
An Important conversation with Mary Purdy
Cleansers, detergents, scrubs, things we use to clean our environments and ourselves may be doing more damage to our health than than they prevent. What about products that go on and in our bodies “ soaps, creams, powders, makeup, body wash, deodorants and anti-perspirants, hair sprays, plastic containers to hold our food in the fridge or microwave. How many products do you come in contact with every day, all days of your life?
And it’s not just the products we use. Disruptive chemicals can be in our clothes or furniture or daily use objects as fire-retardants or easy-clean surfaces.
Mary Purdy is an expert on helping us minimize our exposure to toxins in our environment and maximize our efficiency in ridding them from our bodies, homes, and workplaces.
TRANSCRIPT TO FOLLOW
So, you took a menopause test after dealing with various symptoms and you found out you may be indeed going through menopause. What now?
Well, search on the word “menopause” on the Internet, and where once there was mostly silence, crickets chirping, and the distant sound of an eagle’s cry, now there’s “¦ a lot.
Menopause is having its day, and while that is very good and very overdue, it can be hard to wade through the chaos and separate good information on menopause treatments from rumor and hyperbole. We’ll help you cut through the noise and understand the best menopause treatment options available to you.
If you are looking for treatment options, a Gennev menopause-certified gynecologist can give you a trusted opinion, determine if medication is right for you, and they can provide prescription support. Book an appointment with a doctor here.
Menopause Treatment Guidelines
Menopause is a natural and normal part of a woman’s life, I hear you say. Do we really need treatments for it?
Those lucky few who fly through menopause with nary a hot flash may not need any kind of external support. But many really suffer with menopause vaginal issues, itching, sleepless nights, joint pains, annoying hot flashes, anxiety risks, brain fog, and a host of symptoms that range from disruptive to crippling.
Fortunately, there are treatments and behaviors that can help relieve menopause symptoms, so let’s talk about which menopause treatments work and which don’t, what’s safe and what isn’t.
How can menopause be treated?
At Gennev, we’ve found that menopause treatment follows three general tracks: medical intervention (hormone replacement, antidepressants, etc.), lifestyle and behavioral adaptations (diet, exercise, supplements, alternative therapies), or some combination of the two.
Every woman’s menopause journey is as unique as she is, so the best treatment for menopause for her will generally require a little experimentation and tweaking to get just the right formula.
Medical treatments for menopause
For many women, the safest and most effective menopause treatment is hormone replacement for hot flashes or HRT. While the poorly conducted Women’s Health Initiative trial appeared to indicate that HRT was not safe, the truth is that for most women, if taken correctly, HRT is safe and the best treatment for menopause symptoms.
HRT is the most universally effective treatment for hot flashes and vaginal dryness. In addition, it may provide protection against osteoporosis, heart disease, and even Alzheimer’s disease, so the long-term effects need to be brought in to the risk-benefit analysis.
HRT replaces what your body no longer makes enough of: estrogen. Estrogen does not appear to cause breast cancer (if it did, wouldn’t every woman have it?). However, since it appears to stimulate existant estrogen-sensitive breast cancer, it’s not recommended for women who’ve already had this type of cancer.
Birth control pills and hormonal IUDs help many women with symptoms of perimenopause and menopause. Again, birth control pills or a hormonal IUD like Mirena are not good options for women with a history of estrogen-sensitive cancers, but for many women, the steady release of estrogen can really help balance out hormones during the usually tumultuous perimenopause years.
Antidepressants in low doses can help relieve hot flashes and are generally safe for women regardless of breast cancer risk. The antidepressant dosage recommended for hot flashes is lower than the dose typically used to combat depression.
Moderate vaginal dryness, lichen sclerosus (different than MS), and moderate incontinence can be successfully treated in many women with laser treatments like the Mona Lisa Touch. This is a good, non-hormonal treatment, but it hasn’t been approved by the FDA (though it has been “cleared”). Be sure the practitioner is well-trained in its use and capabilities, and be aware that it is often not covered by insurance.
Bio-identical progesterone creams from a compounding pharmacy are tricky. These are unregulated, so we don’t recommend their use. Additionally, they are no more “natural” than the FDA-regulated medications.
Menopause medicine: over the counter treatments
Taking OTC medicines for menopause can be a bit concerning because lack of oversight from the FDA can mean some products can’t be safely verified. Taking ibuprofen for cramps or to reduce heavy bleeding, or fiber supplements for women’s constipation is probably just fine; getting non-regulated bio-identical hormones from a compounding pharmacy or from the Internet may not be. If you’re going with hormones, please get a prescription from your GP or OB/GYN.
Over-the-counter medications are by nature less powerful than their by-prescription siblings, so you may not find complete or sustained relief. If you’re really suffering, there’s no reason not to get in touch with a menopause doctor near you and get a prescription.
If you have any concerns about your medication, OTC or other, check with your GP, OB/GYN or one of our menopause-specialist telemed doctors.
Natural menopause treatments that really work
First, it’s important to define “natural.” Some define it as “not from Big Pharma.” We understand why women prefer a more natural alternative, but (1) “natural” is not well-defined by any authoritative, regulating body like the FDA, and (2) “natural” does not mean “safe.” Death cap mushrooms are natural, but I wouldn’t want one in my salad.
There are natural remedies that appear to help women, but not enough studies have been done to verify their efficacy. Our approach is, if it doesn’t hurt, and it might be able to help, it’s worth a try. Check out our thoughts on natural remedies in our article “Hot flashes and alternative therapes: What really works?”
Soy (in food, not concentrated supplements, for hot flashes), black cohosh (for hot flashes), Omega 3 (for brain fog and fatigue), vitamin E (for hot flashes), and magnesium glycinate (joint pain, anxiety, and sleep) are all safe and reasonable things to try for menopause symptoms. And any supplement in the Gennev shop has been tested and made to rigorous standards.
Just remember, if you’re adding any concentrated substance to your diet (and this includes supplements, capsules, analgesics, etc.), please check with a doctor who knows your history and what medications you’re on, just to be sure there’s no concern about interactions.
Behaviors and menopause alternative treatments for symptoms
If you’re uncomfortable with hormones or unable to take them, you’re not out of luck. Behavior changes can take you a long way.
Most of these are things you know or can guess; the difficulty is in sticking with them long enough to see real results.
Hydration is so important and will help you more than you can imagine. Your body holds less water now, so dry skin, dry eyes, headaches, fatigue, and brain fog in menopause can all be helped by drinking more. Check out the book Quench by Dana Cohen, MD, if you need more encouragement to hydrate!
Exercise is critical.
Impact exercise like running and walking can help with bones. Building muscles after forty as well as upper body strength can help with retaining muscle and increasing resting metabolism. Core strength can help with balance, meaning fewer falls. And all of these can help lift mood and invite better sleep.
Diet
Diet is another area where a few tweaks can make a significant difference. Now is when you need to increase lean protein and boost healthy greens. The Mediterranean diet is particularly beneficial for women with its emphasis on heart-healthy greens and grains and de-emphasis on red meats. Your brain will benefit, your bones will benefit, and as we age into higher risk of diabetes and heart disease, you’ll have a head start on avoiding long-term illness.
Sleep hygiene
Sleep hygiene is a good idea for everyone, but it’s particularly helpful for peri- and post-menopausal women. Setting a bedtime routine, optimizing your bedroom for sleep, banishing screens two hours before bedtime, going to bed and getting up at the same time every day “ you can start to train your body and mind to understand sleep signals so you can get better rest.
Stress reduction strategies
Don’t just say “yeah yeah” and wave vaguely at the piles of laundry, the bulging work email inbox, the kids, the dog, etc. Yes, life is busy and stressful. No, it’s not healthy, and you need to acknowledge when you need help and a lightening of the load. Taking time for self-care isn’t indulgent or decadent “ it’s critical to good mental and physical health.
If you’re challenged or confused about any of these, or just need an accountability partner, we strongly suggest you sign up for Gennev’s Health Fix. You’ll get unlimited access to our Health Coaches, all of whom are Registered Dietitian Nutritionists and have had special training in menopause care.
There are menopause treatments that really work. It may take some adding, subtracting, tweaking, and testing, but most women find some combination of medical intervention, alternative treatments, and lifestyle change makes them feel a whole lot better.
To find out what route is truly the safest and most effective for you and the menopause symptoms you’re dealing with, talk with a menopause specialist physician. Team up with a Health Coach for ideas and accountability. What’s happening in your body may be frustrating, but it’s normal, and you’re not alone on this journey.
Do you feel comfortable in your own skin?
Many women don’t, and that’s more to do with the expectations we’ve been taught than any real problem with our health or wellness.
Emphasis on women’s outsides has far surpassed focus on a woman’s insides, resulting in a system that has many more solutions for “weight loss” than it does for managing menopause symptoms.
At Gennev, we know the bodily changes that come with aging and hormone declines are natural, normal, and beautiful”they just may not all be comfortable.
So we want to help women embrace a body that may be a little heavier, a little softer, a body that has silver hair and laugh lines to show she’s had a life. We want to help her be comfortable in that body, both by embracing change but also by managing hot flashes and interrupted sleep.

In this podcast, Gennev Director of Health Coaching Stasi Kasianchuk talked with Erica Mouch, a Registered Dietitian Nutritionist who also has a BA in psychology.
Erica advocates and practices from a Health At Every Size® lens in order to support people from all shapes and sizes in healing their relationship with food and their bodies. Erica is also a Certified Intuitive Eating Counselor. Be sure to check out her website, Erica Mouch Nutrition, for more information and to work with her.
Transcript to follow
What are the menopause types and why are they important?
Ask most medical professionals when your menopause transition will start, and they’ll likely give you the same answer: “It depends.”
And that’s true, it does depend on a whole lot of things, including genetics and diet. But it’s not a very helpful answer.
So Gennev’s CEO Jill Angelo and Chief Medical Officer Dr. Rebecca Dunsmoor-Su designed Gennev’s Menopause Assessment to help women be better informed about menopause, where they are in the transition, and how to manage the symptoms.
Your answers to the Menopause Assessment will tell us which of the five Menopause Types you’re in, based on where you are in your Menopause Journey.
Type 1
If you’ve taken the Menopause Assessment and tested as a Type I, probably the most important things to know are (a) yes, some changes are starting to happen; (b) they’re normal and not in your head, and (c) this is an excellent time to start preparing for what’s ahead.
In this phase, your periods are probably changing: you may be experiencing periods coming closer together, with worse PMS and cramping. Later in Type 1, periods can occur farther apart, be heavier, and you might even start skipping some.
You may have gained a pound or two from hormonal weight gain or find it harder to lose the extras that creep on. You may have had some menopause hot flashes, and particularly if you’ve had vaginal births, you may have some urine leakage or urgency. Sleeplessness, mood swings, and low energy are also very common.
Your final period is probably a few years away yet, so you’re in “premenopause” “ your hormones are fluctuating and not always on a predictable monthly cycle.
How we can help
To make life easier, we recommend that you do the following:
- Start or maintain a really good health regimen. The right nutrition, exercise, and sleep habits will make the transition so much easier, but fatigue can make it harder to stay on the right track. We also recommend finding a really good supplement to support your new, healthy habits. Gennev’s Vitality pack for menopause fatigue is formulated for women, filling nutritional gaps as your body’s needs change. Formulated by a naturopathic physician, Vitality is great for sleep, pain relief, immune health, mood, and energy.
Have you tried Gennev’s Vitality Supplement?
Did you know that as women, our ability to absorb nutrients starts to decline at age 40?
Gennev Vitality is a new multi-vitamin supplement for women ages 40+ that’s packed with nutrients that support mood, energy, stress response, immune health, joint pain and inflammation.
- Talk with other women. In the past, we’ve all been discouraged from sharing information about menopause, even with other women! But joining a community of women who have been-there-done-that. Whether it’s increased menopause anxiety or weird, unexplanation sensations, we’ve got you covered! Have a question for a menopause coach or doctor? Join Gennev’s Community forum today.
- Talk with a menopause-specialist OB/GYN to help level out your hormones month-to-month.
- Get a bone density (DEXA) scan to establish a baseline.
- Keep up regular well-woman checks.
- If you have a family history of breast cancer, talk with your doctor about getting on an annual schedule, if you’re not already.
Congratulations on starting your menopause journey informed and prepared! Gennev is here to be your menopause team every step of the way.
Have more questions about Type 1 or menopause generally? Join the conversation on the Gennev Community forum! Haven’t taken the Menopause Assessment yet? Find it here.
October is Global Menopause Awareness Month! Considering how many women enter perimenopause without even knowing it, “awareness” seemed like a good idea to us at Gennev.
So this month, we’re helping women understand where they are in the menopause journey, so they can manage symptoms now and take measures to be healthier in the future.
What is Type 3?
This week, we’re focusing on Type 3, which is typically the first 7 as 10 years of menopause.
Once a woman has gone 12 full months without a period, she’s considered “menopausal.” While periods may be over, unfortunately, some uncomfortable menopause symptoms still remain.
Type 3s, here are your pain points
Congratulations on making it through Type 2! By now, your hormones are beginning to level out (low, but level), and your body has started adjusting to its new normal. Unfortunately, it’ll take some time before you’re fully adjusted, but many things should start to trend better.
Weight
Weight gain has probably slowed as you’re learning how to eat and exercise to fit your new body and metabolism. Ghrelin, the hunger hormone, can spike in some women in perimenopause, but by name it should be coming back under control. Remember that a little extra fat can be protective, so don’t be in too big of a hurry to shed all the weight you may have gained.
Gennev’s solution: Most importantly, embrace your new, beautiful body. It may be softer and rounder, but that’s OK. You’ll want to keep weight under control to ease joint pain and watch belly fat to reduce risk of metabolic syndrome, cardiovascular problems and diabetes, but 30 minutes of exercise a day and a good diet with plenty of water will help.
Hot flashes and night sweats
Hot flashes and night sweats are likely still happening, though they will likely decrease in frequency and severity as you move through Type 3.
Gennev’s solution: If you’re able to take hormones, this is a great time to talk with a menopause-specialist physician about HRT or Hormone Replacement Therapy. Studies are now showing that women who go on estrogen replacement early in menopause reap the most benefits and have the lowest associated risks. If hormones are off the table for you, black cohosh has worked for many women, and our coaches can help you identify lifestyle behaviors that may trigger hot flashes.
Vaginal symptoms
This is the point at which women may begin to experience vaginal dryness and pain with intercourse. As estrogen diminshes, the tissues of the vagina can become drier, thinner, more vulnerable to injury.
Gennev’s solution: Many women find all the relief they need with a good moisturizer or lubricant. Other possible solutions include Mona Lisa Touch treatments, vaginal estrogen, and HRT. Any medication or treatment should be prescribed by a menopause specialist physician to be sure you’re getting safe and consistent dosages of hormones and expert care.
Brain fog
A big factor in Type 3, brain fog and lack of concentration can really frighten women who don’t know it’s coming. Many women have turned down advancement, even quit jobs, or undergone significant tests, fearful they’re experiencing early onset dementia. But brain fog and memory interruptions aren’t unusual as your brain adapts to having less estrogen.
Gennev’s solution: Feed your brain! A Mediterranean diet with its good, lean proteins, leafy greens, healthy fats, and omega-3-rich fatty fishes is a great choice for brain health. Supplementing your diet and filling any gaps in your nutrition with Vitality can help you stay at the top of your game. Make sure you take them with plenty of natural, unadulterated water, which your brain also needs.
Skin and hair changes
As our bodies lose estrogen, we experience changes to hair and skin: both can become drier. Skin wrinkles and loses elasticity, hair grays and thins. Again, it’s good to remember that aging is a privilege denied to many, and our changing bodies reflect a life of experience and wisdom!
Gennev’s solution: While we’re celebrating aging like fine wine, we should also be drinking plenty of water and taking Gennev’s Vitality, which has nutrients that help with the havoc time wreaks on hair and skin.
Musculoskeletal pain
Joint aches are very common”in fact, foot, knee, shoulder, and back pain are some of the most common concerns we hear from Type 3 women.
Gennev’s solution: Keep moving. It might sound strange, but “motion is lotion“ as our Physical Therapy experts tell us. Continuing to move keeps joints lubricated, and it’s that lack of lubrication that causes them to ache in the first place. Also, an anti-inflammatory diet can reduce joint pain, as can magnesium glycinate.
Increasing incontinence
If you’re dealing with mild leakage when you cough or laugh or lift something heavy, or if you find you’re sometimes rushing to make it to the bathroom on time, don’t wait. Incontinence tends to worsen with age, but if you catch it early, incontinence can be halted, even reversed, without surgery. Pelvic muscles, like our muscles generally, can weaken as we age, leading to incontinence and even organ prolapse, so it’s important to strengthen pelvic muscles correctly!
Gennev’s solution: The first best step to dealing with incontinence is to find a Physical Therapist who specializes in the pelvic region. Pelvic PTs can help determine the issue and give you exercises to strengthen pelvic muscles without overdoing it. (Bonus: h3er pelvic muscles = better orgasms.)
Mood swings, anxiety, and depression
In the “good news” category, mood issues tend to dissipate in Type 3 and beyond, so you may be feeling relief from the anxiety, depression, irritability, and rage that can come earlier in the transition.
Still plenty to deal with in Type 3, but as you move through this phase, things should start to improve, and you can focus on the joys of this second half of life. However, it’s time now to consider the long-term effects of estrogen loss, so talk with a menopause-specialist doctor about how best to protect your bones, brain, and heart.
Are you a Type 3, or maybe you have a special Type 3 woman in your life? Come join the conversation about All Things Menopause in our Community forums!
There are no words that capture the weight of 2020. But what I can share after hearing from countless women throughout the year is: You. Are. Amazing!
- 1 million women consumed Gennev podcasts, webinars and articles to learn about symptoms, be supported, and get inspired.
- 100,000 of you completed the Menopause Assessment to learn about your place in the journey.
- 80,000 women joined our community to get informed, work with our menopause team of doctors and dietitians, and use products like Vitality, Magnesium and Sleep CBD to find relief for hot flashes, fatigue, sleeplessness, joint pain, and dryness.
Most of all, you did something. You took charge versus your menopause taking charge of you.
And then there is this from one of our HealthFix members, who shared it with her Gennev health coach this week…
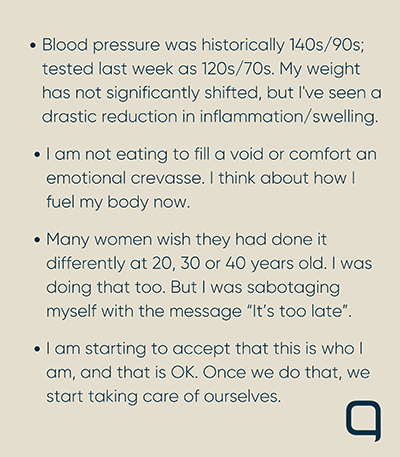
Menopause is hard, but living is in the journey.
When women commit to caring for themselves, and seeking help, they become a force that no one can hold back.
I know because I’m one of them. Like you, many members of our team are in peri/post menopause and we’re building Gennev for you from the vantage point of menopausal women”¦and we love it!
We challenge you to take care of you in the new year as however big or small that may be as you’ve got this, and we’ve got you.
Happy New Year!
Jill
Best of 2020 in Menopause
These are the 5 most read/listened to resources of the year. Enjoy!
10 Important Vitamins for Menopause Relief
Some basics of nutrition really don’t change: veggies are great, you need fat, and eating the rainbow is still a good idea. We updated our list of nutrients that are good for women in perimenopause and menopause, but the basics remain the same.
Thriving Through Menopocalypse With Amanda Thebe (podcast)
Amanda Thebe was a lifelong athlete and fitness enthusiast, but when she hit perimenopause at 43, things went … awry. Fatigue set in, and she found her previously boundless reserves of energy were drying up. And, like so many of us, she didn’t realize right away that the issues she was having were hormonal.
Supplement Savvy With Dr Wendy Ellis
We’re all looking for ways to optimize our health and especially our immunity “ things we tend to take for granted when we’re feeling good and there isn’t a pandemic going on.
Gut Health, Immunity, COVID-19, And Menopause (podcast)
One of the most unknown and underrated ways to strengthen your immune response is gut health. Science is only beginning to understand the importance of a healthy gut, including what all the gut does (a lot) and how best to protect and feed it.
Joint Pain and Menopause: Please Pass The Blueberries
Aching fingers, tight hips, sore knees “¦ joint pain is one of the most common symptoms of menopause. If you’re feeling a bit stiff and sore, especiall
It’s week four of Global Menopause Awareness Month, and we’re continuing our journey through the phases of the menopause transition with Gennev’s Menopause Types.
As we learn more from resources like our Menopause Assessment, we’re discovering there are consistencies in what many women experience. That’s how Gennev was able to develop the five Menopause Types. And women are loving having a tool that helps them understand their bodies better and be more prepared for what may be coming next.
What is Type 4?
Type 4s, that light you see actually IS the end of the tunnel, though at times you might still feel like you’re getting hit by the train. Now several years past your last period, you’re almost ready to throw away that last box of tampons under the bathroom sink, right?
As you move through the Type 4 phase, it’s time to really focus on maintaining your good health for the many happy years ahead. While your body has in many ways adapted to the lack of estrogen, there are long-term effects that require attention.
Type 4s, here are your pain points
By now, hopefully your hot flashes are either gone or clearly going. Your metabolism has likely settled into a new normal, and your weight has, more or less (no pun intended), stabilized. Anxiety, depression, irritability, rage “ those are retreating, and isn’t life more glorious because of it?
It’s good the truly acute symptoms are retreating, so now you can focus on the long-term effects estrogen withdrawal has on sexuality, bones, brain, and heart.
Vaginal symptoms
For many women, vaginal symptoms of dryness and thin, vulnerable tissue can persist for their rest of their lives. Vaginal atrophy can make it hard to want or enjoy intimacy.
Gennev’s solutions: A really good daily moisturizer and intimate lubricant can help tissues stay moister and more pliable. For women wanting to re-engage in sex who find penetration too painful, a series of vaginal dilators or sexual toys can be a huge help.
We also suggest an open dialogue with your intimate partner. Sexual problems can be very damaging to a relationship. Sexless marriage during menopause is common. So, honest conversation, perhaps with professional help, is critical.
Cardiovascular issues
While men do have more heart concerns than women prior to menopause, about 10 years post-menopause, a woman’s risk of heart disease is equal to a man’s. And because we don’t always recognize the symptoms of a heart attack in a woman, her chance of dying of it is greater.
Heart disease remains the #1 killer of women, but it doesn’t have to be. A healthy lifestyle, plus medical intervention when needed, can go a long way to managing and preventing heart disease.
Gennev’s solution: Good nutrition is vital. There are places on earth marked as “blue zones” where people live longer, healthier lives, and centenarians aren’t unusual! Most of those places eat a Mediterranean-style diet, with its emphasis on leafy greens, healthy fats, and lean proteins. Gennev’s Health Coaches are all registered dietitian nutritionists; sign up to get more information on how to eat the way spry 100-year-olds eat!
Exercise, hydration, and social time are also very important. Get your heart rate up just thirty minutes, five days a week. Drink plenty of water. And spend time with friends and family. That’s tough now, with COVID, but studies show those who maintain social relationships as they age just live longer.
Finally, consider a pet. They do the heart and body good “ taking the dog for walks, even just petting and talking to a comfy kitty can reduce stress and increase oxytocin (the “love hormone”).
Brain health
If you looked at that subhead a couple of times and thought, “Who’s Brian?” don’t panic! Brain fog is still common in Type 4, but you should be coming to the end of it soon.
All kidding aside, women do account for two out of every three diagnoses for Alzheimer’s disease, and as Dr. Lisa Mosconi and her team at Weill Cornell Alzheimer’s Prevention Clinic discovered, there does appear to be a connection between menopause, estrogen withdrawal, and development of dementia-related brain plaque.
Gennev’s solution: So how do we protect our brains? Nutrition! As Dr. Mosconi told us in our podcasts with her, nutrition is key: make sure you’re getting plenty of omega 3s (fatty fish”Dr. Mosconi particularly favors caviar), as well as fresh vegetables and fruits, healthy, unrefined oils, good glucose (not just sugar), and plenty of water. Hydration is key, says Dr. Mosconi, as 80 percent of the brain is water! Steeply reduce processed and deep-fried foods, minimize animal products, and stay well away from trans-saturated fats.
If you’re not sure you’re getting enough of any of the good nutrients (and O3s can be particularly challenging if you don’t eat fish), check out Gennev’s Vitality supplement to fill in any gaps you may have in your nutrition.
Bone health
Osteoporosis is extremely common and very dangerous. For one thing, most people don’t know they have bone loss until they experience their first fracture. And since complications from hip fractures kill more post-menopausal women than breast cancer, it’s a real concern.
Gennev’s solution: Obviously, nutrition is huge (again as are you seeing a theme here?) and fortunately, the same things that are good for your brain and heart are also good (or at least not damaging) to your bones: leafy greens, lean proteins, choosing whole foods over processed. Make sure you head to our store to grab vitamin D and Omega 3s and calcium.
Weight-bearing exercise is good for bones, so walking, running, dancing, anything that pits you against gravity is good. And while biking and swimming are great cardio exercises, they don’t help your bones, so try to get some of both. Watch your posture as well! Your body is meant to “stack” so the weight is on your skeleton (which is good for you) and not pulling muscles this way and that (which hurts).
Yes, the years after that final hot flash fades still have challenges, but being proactive and maintaining healthy lifestyle habits can go a very long way. Make an appointment to talk with one of our doctors, and get on the path to thriving through menopause and beyond!.
Some of the best years of your life are ahead of you as enjoy!
Are you a Type 4, or is there a special Type 4 woman in your life? Come join the conversation about All Things Menopause in our Community forums!
The new year has arrived. And whether you consider yourself a “healthy” person or not, January represents an opportunity for new behaviors…or reestablishing old best practices.
Let’s kick off the year with the best of intentions…and actually do them! The team and I at Gennev are doing the same: smarter snacking, revitalize life fitness, dry January…and most of all, booking necessary health & wellness appointments.
Here is the 2021 healthy woman’s checklist…
To your health!
Jill
1. Create a budget
Consider what your health and wellness budget is for 2021. Are you budgeting for self-care? Do you have FSA/HSA coverage through your employer?
If you have FSA/HSA coverage, check to see what it covers in terms of health provider services and products. With a letter of medical necessity from Gennev providers, you can get coverage for appointments, supplements and lubricants on most plans. Here’s a resource for what qualifies for FSA coverage.
2. Book medical appointments
Are you in the practice of annual exams? If not, start now. Book with your physician or with a Gennev doctor.
Have you scheduled your mammogram? If you’re over 45, consider a colonoscopy if you have risk factors in your family. Whatever you do, don’t put the essentials off; talk to a women’s health specialist today.
3. Plan for necessary lifestyle change
Whether you’re in perimenopause or post-menopause, lifestyle behavior change is a must for managing weight, hot flashes, anxiety, sleep, fatigue and joint pain. We know it’s hard, so build a plan for achievable and sustainable change…even if that means baby steps.
Gennev registered dietitians/health coaches work with women of varying levels of discipline, so don’t overthink it, just start doing something. Book an appointment to build a plan for 2021. We believe this will be your best-spent $45 dollars of the year. We want you to thrive!
4. Check your supplement intake
Are you taking the right supplements for your age or stage of menopause? As women, it’s good for us to annually check-in on the supplements we’re consuming “ whether we have the right combination and whether we’re taking them at the right time of day.
If you’re not 100% confident of your routine, start by watching Gennev Director of Health Coaching Stasi Kasianchuk, RDN interview Dr Wendy Ellis about Supplement Savvy. Or – skip to speaking directly with Stasi and her team by booking an appointment with a dietitian (specify that you want a supplement audit).
5. Get the Menopause Guide
We built the Guide to Menopause from the collective expertise of our team of 25 OB/GYNs, naturopathic doctors, registered dietitians and health coaches. It’s a 60-page collection of evidence-based medical, lifestyle and herbal recommendations for every symptom of peri and post menopause. And it’s free. You can’t go wrong.
Type 5s, you are women of mystery!
For the past four weeks, we’ve been defining some of the key stages of the perimenopause-to-menopause journey, helping women locate themselves on the path and take steps to take control of their health. Last week, we took on Type 4.
This week is all about our Type 5s, or as we like to call them, our “Women of Mystery”!
Different factors can make it difficult to pinpoint where you are in your menopause journey. Perhaps you take hormonal birth control pills or have a hormonal IUD. Or you’ve had a hysterectomy that removed your uterus but left one or both ovaries (meaning you’ll go through a menopause hormonally but you’ll have no bleeding signals). An ablation to stop heavy period flows or medications for certain hormonal cancers can also confuse the picture.
What is Type 5?
Type 5 is a general category for women who don’t follow the typical path through perimenopause to menopause. Hormonal birth control may mask many of the symptoms of perimenopause, and since the bleeding that comes during the “sugar-pill” week isn’t a true period, even that doesn’t tell us anything.
Younger women who have certain cancers like breast cancer may even go through menopause twice: once from medicines that suppress estrogen, then again later, as their bodies go through the natural decline of hormones.
If you’re a Type 5, that doesn’t mean something is “wrong” with you. It just means your place in your menopause journey may not be identifiable.
Can I find out my place in menopause?
In some circumstances, you can learn your place in the journey. If you’re on birth control pills, taking a few months off will bring back the bleeding signal (but use some other, non-hormonal birth control!). You can have the IUD removed for the same reason. It may take several months to get a good picture of what your cycle does naturally.
For others, pinpointing their place may not be possible. Stopping medications that help prevent breast cancer recurrence is not a good idea. And for those with ablations or hysterectomy, you may have to depend on other signals, like symptoms.
Some may suggest you get a hormone test to determine your place “ we really don’t recommend that, as results will be skewed by any hormones or hormone-blockers you’re taking. And for those not taking medications, hormone tests still only give a picture of a moment, not an overall view.
Type 5 pain points
Because you’re all over the board, your symptoms are likely to be as well. Or you may not be having significant symptoms because hormones in the Pill or IUD are helping to keep you level.
So it makes sense for you to deal with the symptoms you have and not really concern yourself too much with where you are in the journey. And of course, it always makes sense to do what you need to do to get and stay healthy for the post-menopausal years ahead.
Gennev’s suggestion for you is to start with a consult with one of our menopause-specialist OB/GYNs. A detailed discussion with a doctor who understands menopause and menopause care will shed some light on where you are and why you’re there. Because your situation is unique, a one-to-one conversation about your particular history, health risks, and current experience is necessary. You’ll also get a clearer understanding of your options moving forward.
Depending on your reason for landing in Type 5, you may have different nutritional needs than other women of your same age. If you’ve had cancer, the right nutrition can help you recover more quickly from treatment and even help fight recurrence. Exercise can help you maintain bone and muscle when medications promote bone loss and fatigue “ coaches can help you find activity that you can safely enjoy and keep you accountable to doing it.
Sleep interruption and anxiety are common in midlife, and women who have other health concerns frequently just don’t get the rest they need. Our AM/PM pack are great for promoting better nights so you can have stronger days.
Consider taking a nutritional supplement like our Vitality multi-vitamin pack. Good nutrition is best, but lives are busy and full, and gaps in our healthy eating happen. Vitality can fill in the holes to help you build and maintain a strong immune response.
Yes, Type 5 is its own set of challenges, but like all the other types, Gennev has got your back. Talk with one of our doctors, and get on the path to thriving through menopause and beyond!
Are you a Type 5, or do you have a Type 5 woman in your life? Come join us on the Gennev Community forums, where women share all kinds of useful information and support each other through the challenges!